High levels of testosterone promote energy, drive, ambition, assertiveness, self-confidence, and purpose. Furthermore, high levels of testosterone promote status-seeking (e.g., through buying expensive cars or clothing). Some of this comes down to the way testosterone increases dopamine signaling.
However, testosterone receptors are widely expressed in the central nervous system and testosterone has effects on many brain sites, particularly in “emotional” centers of the brain. Testosterone also affects cognition in poorly understood ways. For example, testosterone improves spatial thinking and women who excel at mathematics on average have higher T-levels.
Of note, it is hard to say which of these effects are caused by testosterone itself, and which are caused by its conversion to DHT or estradiol. For example, if the aromatization to estradiol is blocked the “testosterone”-mediated increase in aggression and libido declines.
Outside the brain, testosterone has a lot of effects on pretty much every bodily tissue, which is the case for many other steroid hormones as well. For example, testosterone strengthens muscles, tendons, and bones. DHT, the primary metabolite, stimulates the expression of the typical “male” phenotype and affects the growth of the larynx, penis, hair, and prostate.
Personal experience
In my early twenties, I dieted down to very low levels of body fat, and my testosterone levels tanked. I jumped on the TRT bandwagon and replaced my testosterone levels for about two to three years. During this time, I experimented with all kinds of combinations of testosterone cypionate, HCG, FSH, and aromatase inhibitors, but the more I tried to mess with it, the worse I felt. Eventually, I settled on the simplest option: testosterone-only (100mg per week) plus a low dose of HcG (125 IU twice per week).
In retrospect, my experience with TRT was quite underwhelming. There was quite a large placebo effect associated with it as I believed that a lot of my problems with my energy, mood, health, and physique could be solved with testosterone replacement – which was simply not true.
Initially, there was a honeymoon period that lasted for a couple of weeks. After that, I have not noticed much of a benefit other than an uptick in drive and an easier time to build muscle.
It did help my physique though. The difference between left and right is roughly 10kg of lean tissue. On the left, my testosterone was borderline low and I have not yet started going to the gym. On the right, my testosterone was at the top of the reference range plus two years of dedicated training (1 hour of gym three times per week). For a picture of me 2 years after TRT with just dedicated training click here and scroll down to the section on “body fat”.

Disclaimer: The right picture was taken right after a gym workout with favorable lighting.
The major thing I noticed was that I needed less sleep, and I was often fine with just sleeping 6-7 hours, an effect I also experience after two weeks plus of semen retention (which interestingly does not affect my testosterone levels but presumably affects ancient neural circuitry upstream of sex hormone signaling).
Another thing I noticed was that testosterone visibly aged me. After a year on TRT, others have commented that my face seems to have grown older by multiple years. This transition from boyish to manly (which is not necessarily bad) may be in part explained by a redistribution of facial fat & a growth in facial musculature but it may also be in part because high levels of androgens drive the aging process.
To some extent, testosterone is like a peacock tail. High levels of testosterone help with signaling “good genes” but at the expense of longevity. Testosterone’s effect on longevity is U-shaped and high levels of androgens are quite bad for every organ system other than the musculoskeletal system and perhaps insulin sensitivity.
Surprisingly, coming off was much easier than expected. I simply stopped injections. After 1 month I was back to my baseline, which is in the 600-700 ng/dl range. Some people have issues with coming off and recovering their natural levels, particularly if they have been using higher doses (e.g., for bodybuilding purposes). Fortunately, I was not one of them.
Thoughts on current trends
Recently, more and more people seem to self-experiment with testosterone. The online landscape paints a picture that a lot of things are explained (and fixed) by the testosterone panacea. From mental health issues, to (lack of) gains at the gym, to motivation and procrastination.
Thus, thousands flock to “TRT clinics”. These clinics are prescription writing factories that will find excuses to give TRT to almost everyone. They make claims that the normal ranges are wrong and the only correct result is to be at the top of, or above, the reference range. They start people on insane beginning doses like 250mg/week because it gives them a rush to feel like it’s “working”.
Spoiler alert: A lot of people are in for a rough awakening…and a prematurely aged body.
Signs & symptoms of low testosterone
- constant low-level background fatigue
- low sex drive
- inability to build muscle
- easily fatigued during exercise
- lack of drive and motivation
- little zest for life
- poor self-confidence
- anxiety and depression
- being skinny fat
- a lot of fat over the triceps area
Diagnostics
- Blood test:
- Minimal: total T, SHBG
- Extensive: total T, SHBG, free T, E2, LH, FSH
- Signs & symptoms
Interventions that worked for me and friends
- Body fat & dieting: In my opinion, the number one overlooked reason for low testosterone is not stress, sleep deprivation, or micronutrient deficiency but caloric restriction or having too little body fat (or chronic dieting). The HPTA axis is quite sensitive to energy balance, particularly leptin levels (discussed here), which makes evolutionary sense. Conversely, having too much body fat also lowers testosterone levels, as adipose tissue expresses aromatase, which aromatizes testosterone into estradiol (E2), which then exerts powerful negative feedback on the HPTA axis.
- TRT: A decent starting dose is 100mg testosterone cypionate per week split into at least three weekly subcutaneous injections (ideally, injecting every day). While I was on TRT I used a low dose of HCG (125IU twice weekly) to preserve fertility and testicular size however, it seems that daily administration is superior (e.g., 50 IU HCG per day). I only ever used insulin syringes and injected into my upper glute area.
- A note on estradiol: One friend, who is a little overweight, is a high-aromatizer. He uses a low dose of the aromatase inhibitor (AI) anastrozole to keep estrogen levels in check (0.1mg twice per week). In my opinion, the vast majority of non-obese people using physiological doses of T do not need an AI, and in fact, may do net harm by adding one. Estradiol is important for many things, from energy levels, mood, libido, cognitive function, and joint and bone and brain health.
- A note on females: Testosterone is very important for women. In fact, molecule per molecule, there is about 10 times more testosterone in women than estradiol. Unfortunately, testosterone is rarely replaced in females, which is a problem for women who take oral contraceptives or women on postmenopausal hormone replacement therapy, both of which have a large shift in their estradiol to testosterone ratio. Therefore, a gynecologist friend gives either DHEA or low doses of testosterone in addition to HRT.
- Avoid: racemic clomiphene (enclomiphene is okay, though very hard to get hold of), most TRT “clinics”, shady over-the-counter testosterone boosters, 19-nor-steroids (which are very suppressive)
Subscribe to the Desmolysium newsletter and get access to three exclusive articles!
A note on blood tests
Blood tests measure what is in the blood. They do not measure cellular action, which is what it is all about. Therefore, when it comes to endocrinology, blood values matter just as much as physical signs (e.g., body hair, heart rate) and symptoms (e.g., fatigue, low libido). This was something that was hard for me to wrap my head around.

Firstly, blood tests only measure hormone concentrations at a specific snapshot in time. For example, simple things such as eating much less for a couple of days will alter hormone levels.
Secondly, blood tests do not necessarily map 1:1 to hormone action because hormone sensitivities differ between people. For example, my testosterone of 600ng/dl is not equal to your testosterone of 600ng/dl (regardless of free levels). Me and you could have different polymorphisms of the androgen receptor (AR). Or we could have different AR densities. Or we could have different versions or amounts of 5-alpha reductase (an enzyme that converts testosterone into the more potent DHT). Or we could have different versions of 3-alpha-hydroxysteroid dehydrogenase (an enzyme that converts androgens into less active metabolites). Or we could have different quantities of androgen-induced changes in transcription factors. Or we could have different accessibility to androgen-sensitive genes. And the list goes on.
All of us have differences in binding proteins, metabolism, cellular sensitivity, function and quantity of receptors, nuclear cofactors, gene methylation patterns, etc. Because of these interindividual differences, optimal hormone levels often differ between individuals – and so do the effects an individual experiences upon the exogenous introduction of a hormone.
All of this makes it seem like blood tests are useless. They are not. Blood tests are highly valuable. However, one needs to keep in mind that, like any other diagnostic test, there are caveats.
It is a mystery why not much research has focused on hormone biomarkers, of which the most promising candidates are probably hormone-specific changes in certain target genes.
Do hormones produce “tolerance”?
The introduction of exogenous hormones is always accompanied by (some) endogenous suppression, which, however, is not the same as tolerance.
Many hormones act on gene expression, either because they act on nuclear receptors (e.g., sex steroids, thyroid hormones) or powerful cytokine receptors directly linked to transcription factors (e.g., leptin, EPO, growth hormone).
Compared to stuff that acts on G-protein-coupled receptors (the targets of most neuropharmaceuticals or recreational drugs), there is much less tolerance to these direct changes in gene expression, which is the most downstream level possible.
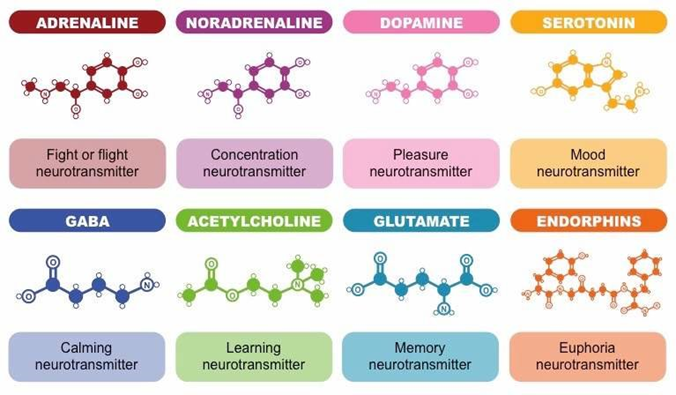
However, there will be some tolerance to some effects on neurotransmitter systems (which is what many people are after). For example, after starting testosterone, many experience energy, motivation, and even slight euphoria. These effects are mostly due to testosterone affecting neurotransmitter systems, particularly the dopaminergic system.
Unfortunately, changes in neurotransmitter systems and the ensuing “honeymoon period” are somewhat short-lived. After raising the dose, individuals will often “feel” much better for a short period of time (usually on the order of weeks). However, after a couple of weeks, the brain-based hedonic treadmill takes over and neurotransmitter signaling drifts back toward baseline.
Unfortunately, “how we feel” is not the best guiding factor to determine hormone dosages. “How we feel” depends entirely on the nervous system and we do not “feel” whether the liver, heart, kidney, immune system, etc. are in a hypo- or hyperhormonal state. Therefore, hormones should not be dosed solely depending on “how one feels”.
Hormone tunnel vision
If hormone levels are low, then replacing the hormone in question in a balanced way is a safe, causal, and effective way to rectify the symptoms associated with hormone deficiency. However, it seems that many people are chasing symptoms (e.g., libido, energy levels) and end up replacing hormones in supra-physiological doses even though the putative hormone deficiency was not the root cause of their symptoms in the first place.
For example, guy X might be somewhere around the 40th-50th percentile of testosterone levels. He believes he has every low-T symptom under the sun including fatigue, difficulty losing weight, poor self-confidence, low libido, etc. He is dead certain that his low testosterone levels are at fault for his symptoms and self-diagnoses with “low T”.
Guy X starts to replace his testosterone. Dopamine levels rise and he feels great for a couple of weeks. He believes that he has found the root cause. But as his dopaminergic system adapts, he is soon back to square one. Now the raise, raise, raise period begins, during which he always feels good for some time after every raise, assuming he has simply not raised his dosage enough, even though his levels of testosterone are far above the normal range already.
Gradually he starts to feel “like shit” again. Now he starts to blame the rising estrogen levels. He titrates back and forth testosterone and aromatase inhibitors, assuming he simply has not found the holy balance yet.
However, testosterone was never his issue to begin with and the initial ‘Low T’ problems come back after the honeymoon period. The issues are often complex processes in the nervous system, which might be unrelated to hormone levels. Quite often, the root cause is undiagnosed low-level dysthymia or depression (which is not the same as “suffering”).
If one’s issue is primarily of neurotransmitter or central origin, replacing hormones can definitely bring about (temporary) improvement, particularly replacing hormones in supraphysiological doses in order for them to have supraphysiological effects on various neurotransmitter systems.
Nonetheless, in these cases, hormone replacement is not addressing the root cause and improvement will be incomplete and temporary, even though people can often feel much better over a short period of time.
Abusing hormones for symptom relief is not just unhealthy, but can be quite dangerous and cause irreversible changes in a number of organ systems. Furthermore, it is trading in short-term vitality for long-term health.
Unfortunately, the symptoms of hormone deficiencies overlap with the symptoms of low-level depression and other conditions that are only weakly related to the endocrine system.
In fact, many people with symptoms of hormone deficiencies (e.g., fatigue, low energy, bad sleep, anhedonia,) do have low-normal hormone levels. Some people choose to replace hormones, only to find that it does not bring lasting relief. The meteoric rise in TRT is just one example.
In my opinion, many people would be much better off in terms of safety, health, efficacy, and reversibility if they made major changes to their lifestyle or interfered with neurotransmission directly. For example, I know of two people who switched from testosterone replacement therapy to bupropion, with better and more sustained effects on energy, mood, motivation, and sex drive – the reason why they sought testosterone replacement therapy in the first place. Furthermore, bupropion is leaving most organ systems untouched that would be adversely affected by testosterone.
In sum, some people fare better with antidepressants. As always, the drug regimen of choice is best found through cautious empirical self-investigation.
This last part was an excerpt of my article on the “basics” of hormones – The Life-changing Power of Hormones, which I recommend reading if hormones interest you. Among other things, I discuss why hormones are so powerful, why hormones are underused, strategies to optimize hormones naturally, why blood tests are often misleading, hormone cross-talk, and hormone tunnel vision.
Part II: My TRT Lite Protocol
I have experimented with TRT a second time and I am still on a modified version of it. For more: My TRT Lite Protocol
