Cortisol is a very misunderstood hormone. While chronic cortisol excess has degenerative effects on every bodily tissue, cortisol deficiency makes people feel miserable, including brain fog, lack of motivation, abysmal energy levels, “feeling like shit”, and weakness.
Out of all the hormones occurring in the human body, cortisol is the most motivating and stimulating. Cortisol gives energy, vitality, and “punch”. It clarifies thinking, sharpens concentration, and improves cognition & memory, giving a “clear” head and a sharp mind. Furthermore, cortisol increases the availability of plasma nutrients and regulates the immune system. All of this makes physiological and evolutionary sense in times of stress and danger.
The right level of cortisol is vital for performance and well-being. In fact, low cortisol is a surprisingly common but somewhat underappreciated cause of low energy levels and brain fog. Thyroid hormones regulate the “idle state” while adrenal hormones are the “gas pedal”. Both are needed for good energy.
Replacing cortisol in a cortisol-deficient person has quick and dramatic effects. Therefore, hydrocortisone is thought to be a viable option for the (temporary) treatment of burnout states, and chronic fatigue syndrome. Furthermore, the use of corticosteroids can help atypical depression and kinds of depression that are due to “sickness behavior”. However, hydrocortisone is powerful, and its use can be quite dangerous, degenerative, and pro-aging.
Anecdotally, there are whole underground communities of people who have “got their life” back by implementing low-dose cortisol replacement regimens. Reportedly, some people have been taking supplemental cortisol for many years without (major) issues – though they may artificially accelerate their rate of aging and other degenerative conditions.
Of note, people in the military and other high-energy jobs often have SNPs that are associated with hypercortisolism. These people overproduce cortisol, have a lot of energy, can pull all-nighters easily, and age quickly. I discuss the effect of cortisol on aging in more detail here.
Personal experience
In my early twenties, I was battered by “adrenal fatigue”, which has little to do with the adrenals but everything with the hypothalamus (and should therefore be called “HPA-axis dysfunction”). It is due to the hypothalamus not sending enough signals (CRH) not sending enough signals to the pituitary, which then sends insufficient signals (ACTH) to the adrenal glands.
My low levels of cortisol were brought about by undereating, intermittent fasting, and buying too much into “health” advice. At my worst, I felt like absolute crap. I needed to exercise vigorously every day in order to feel and function well.
Because my symptoms matched my symptoms of cortisol deficiency, I decided to give it a try. Already on my first dose, it gave me a lot of mental and physical energy.

It was particularly helpful for studying. Even low doses sharpened my thoughts, clarified my thinking, improved my memory, and killed any brain fog – all of which make physiological and evolutionary sense in times of stress.
For a couple of months, I continued to supplement with low doses of cortisol, with great effects. Because I kept doses low, I have not noticed any negative effects on my metabolic health or other aspects. As my HPA-axis reregulated, I tapered off. After a month or so, my endogenous cortisol levels recovered to normal levels, as judged by bloodwork and symptoms.
After having recovered, the effects of supplemental cortisol had diminished to the point of being negligible. In fact, if I now take HC I barely feel anything whereas before even small doses were quite stimulating.
I mostly used cortisone acetate (the inactive form of cortisol) instead of hydrocortisone (the active form), which allowed for the area-under-curve tissue cortisol levels to be lower (higher cortisone to cortisol ratio), possibly making cortisol replacement a little safer. Furthermore, because cortisone needs to be hepatically activated to cortisol first, cortisone acetate has a slight extended-release effect.
Over the last couple of years, I would turn to low doses of hydrocortisone or cortisone acetate occasionally whenever I wanted or needed to be at my best. Usually in low sublingual doses (2.5mg), which are quick-acting (within 30 minutes). In my experience, cortisol feels very natural and has no counterregulation or comedown. However, whenever I took it at night, my sleep took a hit, and I woke up earlier than usual.
Cortisol is unique in that it does not “distort” the balance of neurotransmitters, quite similar to the after-effects of ketamine. It just made me more “me”. Therefore, I sometimes used a low dose of cortisol before a first date, though eventually, I stopped doing that because it removed my filter of whether a girl excited me or not.
At low dosages (e.g., 2-5mg) and if used occasionally, cortisol is mostly safe in the same way that vigorous exercise or a cold shower is mostly safe, which also spikes cortisol secretion temporarily. However, at higher doses, cortisol is far from safe, as discussed shortly.
A good friend of mine says that dosages as low as 3mg can stimulate him for many hours. He claims that out of all of the things he had ever tried, temporary cortisol replacement was the thing he benefitted from the most, and to this day he is taking 5mg of hydrocortisone in the morning.
For reference, daily production in a healthy, young, active male is about 20-30mg per day – with lots of interpersonal variance.
Another friend noticed that when he takes supplemental cortisol, he now wants stress and challenges and he becomes a borderline drama queen. It is no coincidence that individuals with borderline personality disorder usually have elevated cortisol levels.
Signs & symptoms of low cortisol
- abysmal energy levels
- dark under-eye circles (because of low sympathetic nervous system activity)
- brain fog
- difficulty waking up
- exhaustion at night
- over-reliance on caffeine
- low blood pressure
- dizziness upon standing up
- sugar & salt cravings
- low body temperature
- difficulty adjusting to changes in ambient temperature (especially heat intolerance)
- scanty perspiration
Diagnostics
- Diagnosing low cortisol is hard. Unfortunately, blood tests, urine tests, or saliva tests are only moderately useful. DHEA-S is an okay marker of total adrenal output. 24-hour urinary cortisol is semi-valuable. Morning-free cortisol and 4-point saliva tests are probably the most valuable.
- Signs & symptoms (see above)
- Trial dose of hydrocortisone – If one can really “feel” a very low dose of exogenous cortisol, it is likely that the person has low baseline cortisol levels.
Intervention that worked for me and friends
- Rhodiola or ashwagandha for light „adrenal fatigue” (i.e., HPA-axis dysfunction)
- Licorice root (inhibitor of HSD-II enzyme): HSD-II converts cortisol to the inactive cortisone. Even though effective, it is presumably unsafe. When I was taking it, my aldosterone levels were suppressed to the point of being unmeasurable and my 24-hour urinary cortisol profile was drastically elevated, possibly exposing my kidneys to large glucocorticoid loads.
- Lifestyle: stress reduction, sunlight & bright light therapy (especially in the morning), eating enough calories
- Falling in love: Individuals who have recently fallen in love show a drastic increase in cortisol secretion (about 40%) for up to 6 months.
- Specific antidepressants: bupropion, vortioxetine, moclobemide
- Last-line: cortisol replacement therapy.
- Avoid: intermittent fasting, ketogenic diets, caffeine, expensive “adrenal fatigue” supplements or doctors
How it works
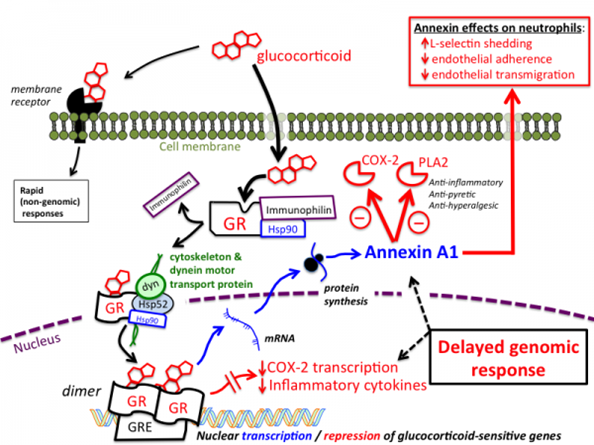
Cortisol is a steroid hormone, affecting every single nucleated cell in the body (i.e., all cells other than red blood cells and platelets). Cortisol (like testosterone or thyroid hormones) modulates the expression of thousands of genes in every single cell in a vertebrate body. In this lies its unique power (and also its danger). I discuss hormones in more detail here.
The purpose of cortisol is to prime the body and mind for action. Whereas almost every stimulant in existence acts on measly transmembrane receptors, hydrocortisone acts on nuclear receptors, to which counterregulation does not apply (or only very little).
Physiological doses of cortisol have a variety of effects on the body and mind:
Cortisol boosts the release of a variety of neurotransmitters, first and foremost dopamine. Cortisol is perhaps the most powerful hormone in terms of regulating baseline dopamine levels – even more powerful than testosterone. Furthermore, cortisol potentiates intracellular dopamine signal transduction. It also upregulates dopamine receptors. Similar things hold true for noradrenaline.
For example, after removal of adrenal glands, D1 receptor expression falls by about 40%. Furthermore, very high levels of glucocorticoids can lead to euphoria (“steroid euphoria”) and rarely even lead to mania and psychosis (”steroid psychosis”).
Because cortisol increases catecholamine neurotransmission, when cortisol levels are high (whether pharmacologically or naturally), every other stimulant is potentiated. Conversely, if cortisol levels are low, other stimulants do not work as well. Similar things hold true for thyroid hormones.
The increase in glutamate and catecholamine transmission increases the intensity of felt emotions (and may therefore improve anhedonia). In fact, hypercortisolism leads to an emotional rollercoaster. It is no coincidence that patients with borderline disorder seem to have an overactive HPA axis.
Cortisol also acts on a variety of other brain sites.
At medium to high levels, cortisol is great stuff for the hippocampus and few other drugs or hormone are as powerful in promoting cognition and memory formation, which makes evolutionary sense. Conversely, at high levels for an extended time, it is toxic – probably due to glutamatergic excitotoxicity and cellular anti-repair/catabolic effects.
Similarly to how cortisol affects the hippocampus, cortisol also has powerful activating effects on the amygdaloid bodies and the prefrontal cortices in the short term (days to weeks). However, over long periods of time (months) the hippocampi atrophy, the amygdalae hypertrophy, and the prefrontal cortices undergo adverse microarchitectural changes, making people more stressed, less rational, and more stupid.
Interestingly, giving people a single dose of HC after a traumatic event can prevent many cases of PTSD, in part, because CRH-signaling is turned off by a negative feedback loop, which then (presumably) prevents the formation of “flashbulb memories”.
In terms of physical effects, in the short term, cortisol activates the whole nervous system in a similar way to stimulants. It increases muscle strength, suppresses appetite, sharpens concentration, and increases plasma nutrient availability. Many athletes were known to abuse it, especially in cycling. Understandably, it is banned by WADA.
In the long run, excess cortisol is very catabolic to pretty much everything leading to muscle atrophy, osteoporosis, paper-thin skin, and organ degeneration (including the brain). As a doctor, I sometimes see patients who have been taking pharmacological doses of glucocorticoids (e.g., 5mg of prednisone) for many years. They often have terrible and easily bruising skin, central obesity, and thin extremities. Sometimes they develop cataracts. Blood pressure and blood sugar are usually poorly controlled. Pretty much without exceptions, these individuals look 10-15 years older than they are.
Psychiatric symptoms such as insomnia, depression, anxiety, easy irritability, paranoid episodes, and attempted suicide or panic attacks are present in more than half of patients having any cause of Cushing’s syndrome – usually without the patients being aware that their “psychological” issues are mostly caused by a primary biological aberration.
So in sum, in the short term cortisol gives a lot of energy and amazing brain function. In the long term, high doses of cortisol degenerate everything.
Nuclear receptors are not the whole story
Whenever I took hydrocortisone sublingually, I was stimulated within a couple of minutes. However, this was long before any meaningful gene expression could have occurred. It turns out that next to conventional signaling via nuclear receptors (which takes around 30–60min to show effects), there are also membrane glucocorticoid receptors (mGRs), which are GPCRs.
These “classical” membrane receptors mediate many of the rapid effects of glucocorticoids in the early stress response via modulating neuronal activity in the hypothalamus, hippocampus, amygdala, and prefrontal cortices, among other areas.
The danger of glucocorticoids
Cortisol is a powerful hormone, and its use can obviously be dangerous. At high doses for a long time (months to years), high levels of cortisol can have hardly reversible negative effects on brain function and structure, regardless of whether these levels are induced naturally or pharmacologically.
For example, at high levels, cortisol induces nerve cell death in the hippocampus, which has a great density of glucocorticoid receptors, while there is synaptic growth and an increase in amygdala size. Furthermore, cortisol negatively alters the neuroarchitecture of the prefrontal cortices, generally having atrophying and degenerative effects.
Together, these changes can cause depression and insidious cognitive decline in the genetically vulnerable.
Furthermore, if used incorrectly, glucocorticoids can cause osteoporosis, muscle loss, Cushingoid fat distribution patterns (e.g., moon face, buffalo hump, truncal fat, thin extremities), metabolic syndrome, insomnia, depression, dementia, high blood pressure, and premature aging.
These changes are not like normal drug side effects, which occur in a single-digit percentage of people. Most of these effects will occur in pretty much everyone who is exposed to high enough levels of glucocorticoids for a long enough time.
Furthermore, the amount of cortisol someone produces is one of the many variables determining how fast someone ages. At high doses/levels, cortisol has pro-aging effects on every cell of the body because cortisol changes the expression of a number of genes involved in cellular repair, growth, and autophagy.
This is part of the reason some females seem to have aged five or more years over the course of a single pregnancy, a time during which cortisol levels are double to quadruple their normal levels.
Speculatively, this may have also been part of the reason why the body of 39-year-old MLKJ reportedly looked like the body of a 70-year-old during autopsy. Due to the intense pressure he was under, his adrenals have probably been secreting vast amounts of cortisol for years.
There is a reason for the saying that “stress can kill you”. Well, it is not the “stress”, but rather the associated hypercortisolemia.
For example, let’s consider the two species of prairie voles who are closely related but have a very different lifespan. It turns out that one of these species lives in a habitat with much more predation, therefore having evolved a much greater cortisol secretion. Cortisol gives physical energy, mental alertness, and nutrient mobilization, all of which are beneficial in times of stress (or in a stressful environment). However, at high doses/levels, cortisol has pro-aging effects on every cell of the body due to changing the expression of a number of genes involved in cellular repair, growth, and autophagy. It is hypothesized that the different rates of cortisol secretion account for most of the different aging rate of these species.
Thoughts on “adrenal fatigue”
A lot of people lump a couple of different pathologies under the umbrella term “adrenal fatigue”. These include true “adrenal fatigue” (which has nothing to do with the adrenals but, as mentioned, is a hypothalamic issue), hypothyroidism, and a low noradrenergic tone.
All of these syndromes present with a very similar set of symptoms, such as heat intolerance, an inability to sweat, “feeling like shit”, feeling burnt out, needing coffee to survive, hypoglycemia, dizziness, and a low heart rate and blood pressure.
Furthermore, “adrenal fatigue” is hard to differentiate from atypical depression. For example, both have a blunted HPA axis, chronic low mood, fatigue, sleeping in, salt & sugar cravings, laying around all day, and being overly sensitive. And both will improve if hydrocortisone is given. Even though there is some etiologic overlap, these different syndromes need to be approached very differently.
What “label” someone will be diagnosed with depends in part on what kind of specialist people see (whether a naturopath or a psychiatrist). I discuss atypical depression in more detail here.
Other experience reports
For a full list of experience reports, including non-stimulants, click here.
Sources & further information
- Opinion article: Dr. Linder – Cortisol
- Scientific article: Endocrine Aspects of Burnout
- Scientific article: A Review of Hypothalamic-Pituitary-Adrenal Axis Function in Chronic Fatigue Syndrome
Disclaimer
The content available on this website is based on the author’s individual research, opinions, and personal experiences. It is intended solely for informational and entertainment purposes and does not constitute medical advice. The author does not endorse the use of supplements, pharmaceutical drugs, or hormones without the direct oversight of a qualified physician. People should never disregard professional medical advice or delay in seeking it because of something they have read on the internet.
