I find that life is much easier and much more enjoyable if I have great energy levels, mood, and health. In fact, whatever I want in life, great vitality is perhaps the most important requirement to get me there.
As it turns out, my vitality is closely dependent on my hormonal balance. If even one of my major hormones is off, my vitality takes a severe hit, and no lifestyle intervention, supplement, or drug can remedy that.
Conversely, I was more vital, energetic, and emotional during puberty, a time during which most of my major hormones were at their peak, and there is in part a causal connection.

Many of the major hormones affect every bodily system because they modulate cellular gene expression directly – the deepest and most powerful layer of intervention.
My experiments and experiences with hormone replacement lead me to believe that a non-minor subset of people who have to rely on stimulants to function and be productive may simply have low levels of testosterone, cortisol, thyroid hormones, leptin, or a combination of these.
Experience reports for individuals hormones:
Some general stuff about hormones
Life consists of cells. Cells are biological machines emerging from the laws of chemistry and physics and just do what they are programmed to. The blueprint for this program is written in the form of the genetic code.

A multicellular organism relies on the different functions carried out by its many different specialized cells and each cell contributes to and benefits from homeostasis, whose ultimate point is survival and reproduction of the organism. For the coordinated function of these many different cells, systemic coordination is necessary.
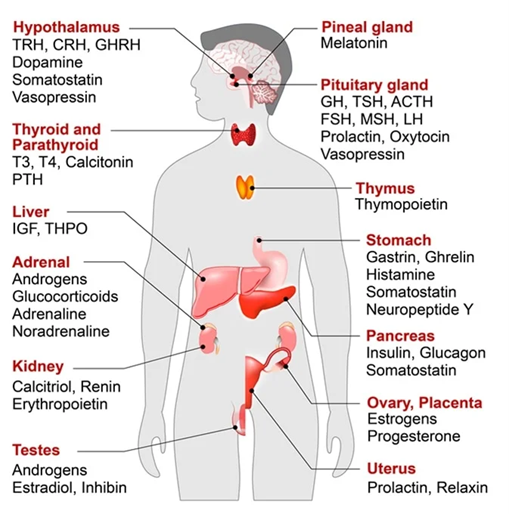
Multicellular organisms evolved signaling molecules to coordinate the activity and behavior of the different cells separated by a distance. Next to local small-scale coordination via paracrine mediators, there are certain signaling molecules that are used for large-scale coordination of many different cells, tissues, and organs at the same time. These systemic signaling molecules are called hormones.
Some of the major hormones, including steroid hormones (e.g., cortisol, estradiol, testosterone), thyroid hormones, and IGF-1 act on pretty much every cell of the body at the same time. By acting on the blueprint written in the form of the genetic code, these hormones instruct cells on a body-wide level how they should behave.
For example, insulin signals to store nutrients and regulates metabolic flux, thyroid hormones determine the metabolic rate, sex hormones instruct the organism to get ready for reproduction, IGF-1 induces growth and repair, cortisol instructs cells to prepare for stress, etc.
Many of the major hormones achieve this systemic coordination by directly affecting gene expression (among other things) and are therefore among the determinants of what programs -and to what extent- are running in any given cell at any given point in time.
With very few exceptions, almost every single cell in the human body has millions of receptors for all of the major hypothalamic hormones (sex hormones, stress hormones, growth hormone, thyroid hormones).
Each of them unlocks a specific portion of the genetic code, depending on what part of the code is accessible, which differs between tissues. This is what makes hormones uniquely powerful – far more powerful than a pharmaceutical drug merely affecting a single target.

Each of the major hormones affects each single cell in multiple ways.
- Firstly, as explained above, many hormones have direct genomic effects that alter the expression of the genetic code, sometimes in major ways. For example, testosterone causes the expression of hundreds of genes that have the androgen response element in their promoter region. The expressed proteins then alter cellular function in testosterone-specific ways, such as hypertrophy in muscle cells, maturation in sperm cells, or an increase in the activity of dopamine-producing neurons.
- Secondly, hormones have indirect effects because each hormone affects many other hormones and mediators. For example, testosterone affects levels of cortisol, insulin, leptin, oxytocin, and IGF-1, which each then have effects on their own.
- Thirdly, hormones affect energy levels, mood, and health and therefore have a major influence on behavior, which then affects the lifestyle choices people make, which then affects the whole body in a number of ways. For example, testosterone increases energy levels, motivation, and stimulates musculoskeletal changes, which then affect the desire and ability to exercise.
As may be evident by now, if one of the major hormones is off, this will have major effects on the whole organism, ranging from genome, cell, tissue, organ, physiology, behavior, and life situation. Conversely, hormone therapy is perhaps among the most holistic therapies currently available – holistic in the sense of affecting all aspects of the body and mind.
While the mechanism of action of most pharmaceutical drugs is usually high upstream in the signaling hierarchy, many hormones act at the most downstream level possible (gene expression) affecting the whole organism from deep within. Each of the major hormones modulates every bodily system, having powerful effects on the cardiovascular system, immune system, musculoskeletal system, liver, kidneys, brain, etc.
In my opinion, using these natural molecules my body had been adapted to for millions of years is more “natural” and more effective (and presumably also healthier) than the current medical practice of sick care (instead of health care) to prescribe a cocktail of different drugs to patch up all the individual symptoms, complaints, and every abnormal physical or laboratory finding separately.
For example, hypothyroidism is associated with fatigue, depression, weight gain, and dyslipidemia. Often, these symptoms are patched up individually with caffeine, antidepressants, metabolic drugs, and lipid-lowering agents.
Why are hormones underused?
Diet, exercise, sleep, stress reduction, and connection with others are all important for living a long and healthy life. But few things have as profound an immediate impact as restoring hormones to optimal levels.
Unfortunately, hormones are something doctors rarely properly look at, and hormone replacement therapy is rarely used by most doctors. In fact, many doctors are scared of it. In my experience, most doctors would rather prescribe a cocktail of unnatural drugs instead of the necessary bio-identical molecules. I suspect that this is mostly industry-driven.
Speculatively, hormones are widely neglected by mainstream medicine in part because the evidence for these natural molecules is quite poor (however, absence of evidence is not evidence of absence). The medical system is a huge industry and as is the case with other industries, it depends on revenue generation (“follow the money”).
Most revenue is made from patents. However, hormones are natural molecules, which nobody is allowed to patent. Therefore, since not much money can be made from hormones, they do not have as much evidence behind them as pharmaceutical drugs, given that a lot of evidence generation is funded because of financial incentives.
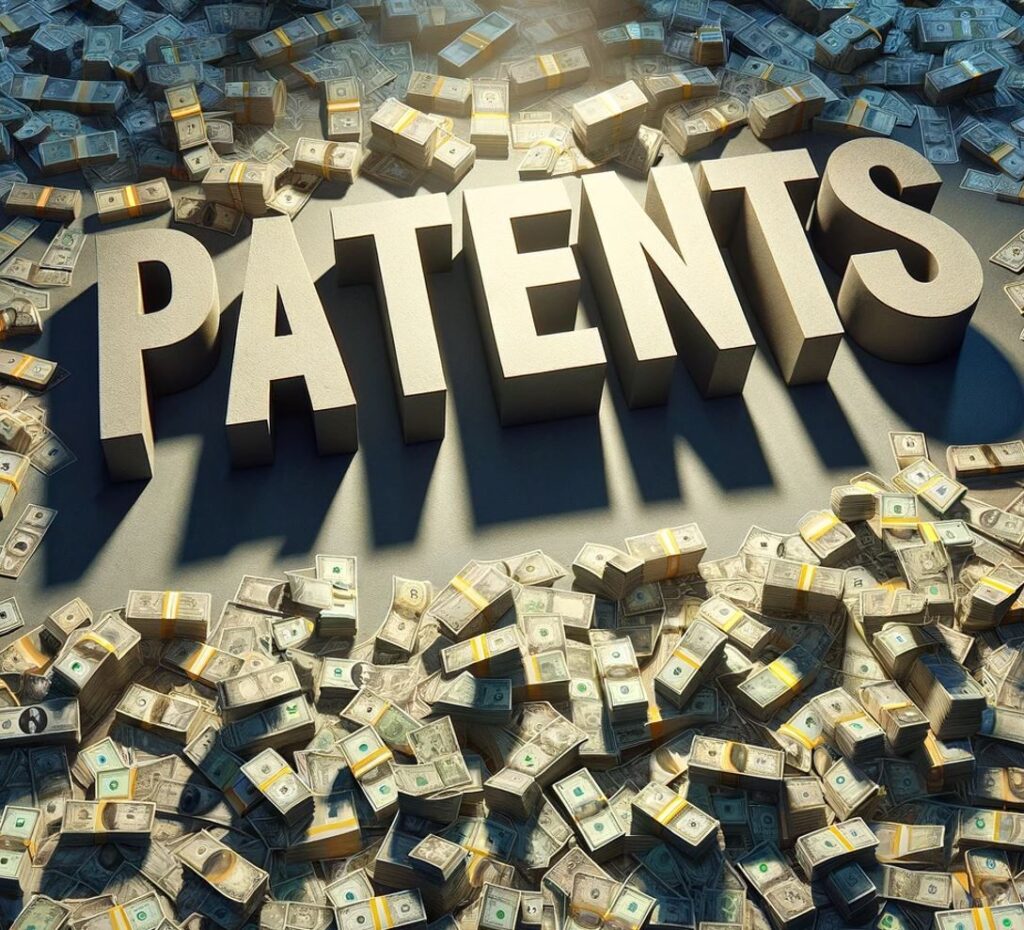
The evidence-generation process is a revenue-generation process, distorting medical science so much that many physicians have unfounded confidence in unnatural drugs while remaining ignorant and fearful of natural hormones.
Even though not (yet?) widespread, the use of hormone therapy is no secret, and many doctors around the world have recognized their unparalleled power. The focus of these doctors is often on prevention and longevity, trying to keep the patients healthy and functional for as long as possible instead of being financially incentivized by sickness.
Many of these doctors use hormones extensively and have been doing so for decades in thousands of patients. They often balance multiple hormones simultaneously using small physiological dosages. There certainly are risks (as there are with any other therapy) but if doses are physiological, hormones properly balanced with each other, and the proper delivery route used, the risk is much smaller than what conventional medical “wisdom” leads people (and doctors) to believe.
For a long time, many of these doctors have practiced in the background, largely outside the established medical system, and predominantly served the rich and powerful, though it seems that times are changing.
Hopefully, proper hormone replacement will be more widely accessible in the future beyond the domains of “alternative”, “functional”, “complementary”, or anti-aging medicine.
Unfortunately, many people do not like hormones because they prefer “natural” treatment instead. They would rather ingest truckloads of unnatural herbal supplements than administer the natural hormones our physiologies evolved with for millions of years.
Personal experiences
Over the years, I have experimented with a large number of hormones. Feel free to click on the links below to read about my experience in more depth.
The difference between “transformative” and “supplementary” hormones do not relate to the general importance of a particular hormone but rather to how much a hormone has changed my life at the point in time I experimented with it. All the “transformative” hormones have been life-changing in one way or the other and I would not be today where I am now without them. Conversely, all the “minor “supplementary” hormones were interesting but not life-changing in any way.
Transformative hormones
Supplementary hormones
- Growth hormone
- Insulin
- EPO
- Estradiol
- Oxandrolone
- Oxytocin
- ADH
- Pregnenolone
- DHEA
- Teriparatide
I will publish articles about these supplementary hormones soon. To get notified when they are available, sign up for my newsletter.
Subscribe to the Desmolysium newsletter and get access to three exclusive articles!
Strategies I follow to optimize my hormones naturally
- I optimize my sleep.
- I make sure I eat enough calories (for me, about 3500-4000kcal per day), with enough good carbs and good fats. Whenever my caloric intake is insufficient, some of my hormones decline, including sex hormones, thyroid hormones, and IGF-1.
- I stopped any kind of fasting (both multi-day fasting as well as intermittent fasting) in part because fasting can cause all sorts of hormonal issues.
- I put a prime on exercise – but I make sure not to overdo it.
- I used to make sure that I do not dip below 14% body fat. Whenever I did, a number of hormones took a hit. Starting semaglutide allowed me to tolerate about 2% lower levels of body fat without hormonal deterioration. I now circumvent this problem altogether by taking a low dose of metreleptin sufficient to mimic a body fat percentage of about 15-20% (but without the aesthetic and metabolic downsides). The last time I checked, my body fat percentage was 10.6% (DEXA).
- I take a couple of supplements to prevent nutrient deficiencies (discussed here).
- I run an extensive hormone panel once per quarter (discuss here).
I discuss hormones & aging in more detail here.
Hormone deficiencies often go unrecognized
A non-minor number of individuals are hormone deficient. A large number of external or internal conditions can cause endocrine imbalances. These include insufficient food intake, lack of sleep, excessive exercise, fasting, ketogenic diets, low body fat percentage, immune system issues, nutritional deficiencies, high stress levels, or “healthy things done in excess”.
Quite often, people go doctor-shopping but they often cannot find anything. There are two primary reasons for this:
- The specializations and subspecializations in medicine have produced many doctors who are blind to everything out of their narrow domain and therefore hormones are rarely properly checked.
- Lab values often come back “normal” and therefore many hormone-deficient patients fly under the radar of the current medical system of doctors who just look at values that are flagged.
How to check for hormone deficiencies?
All of the major hormone deficiencies (thyroid, sex hormones, cortisol, leptin, growth hormone) have partially overlapping signs and symptoms. These include fatigue, low mood, low libido, bad sleep, brain fog, low motivation, and weight gain, and sometimes even anxiety or depression. However, these signs and symptoms are shared with many other non-hormonal conditions as well.
Because symptoms are often unspecific, getting a decent hormonal panel is a reasonable starting point.
Here is what I would test for:
- TSH, fT3, fT4 (optional: reverse T3)
- Total testosterone, SHBG, estradiol (free testosterone can be calculated from total T & SHBG & albumin)
- DHEA-S (a marker for adrenal status)
- IGF-1 (a marker for nutritional status & growth hormone secretion)
- Leptin
- Vitamin D (yes, vitamin D is a hormone as well)
Then, in combination with test results, going through the signs & symptoms of a specific hormone deficiency. Some of these signs & symptoms were listed above.
A note on blood tests
Blood tests measure what is in the blood. They do not measure cellular action, which is what it is all about. Therefore, when it comes to endocrinology, blood values matter just as much as physical signs (e.g., body hair, heart rate) and symptoms (e.g., fatigue, low libido). This was something that was hard for me to wrap my head around.

Firstly, blood tests only measure hormone concentrations at a specific snapshot in time. For example, simple things such as eating much less for a couple of days will alter hormone levels.
Secondly, blood tests do not necessarily map 1:1 to hormone action because hormone sensitivities differ between people. For example, my testosterone of 600ng/dl is not equal to your testosterone of 600ng/dl (regardless of free levels). Me and you could have different polymorphisms of the androgen receptor (AR). Or we could have different AR densities. Or we could have different versions or amounts of 5-alpha reductase (an enzyme that converts testosterone into the more potent DHT). Or we could have different versions of 3-alpha-hydroxysteroid dehydrogenase (an enzyme that converts androgens into less active metabolites). Or we could have different quantities of androgen-induced changes in transcription factors. Or we could have different accessibility to androgen-sensitive genes. And the list goes on.
All of us have differences in binding proteins, metabolism, cellular sensitivity, function and quantity of receptors, nuclear cofactors, gene methylation patterns, etc. Because of these interindividual differences, optimal hormone levels often differ between individuals – and so do the effects an individual experiences upon the exogenous introduction of a hormone.
All of this makes it seem like blood tests are useless. They are not. Blood tests are highly valuable. However, one needs to keep in mind that, like any other diagnostic test, there are caveats.
It is a mystery why not much research has focused on hormone biomarkers, of which the most promising candidates are probably hormone-specific changes in certain target genes.
A note on reference ranges
Most doctors are trained to recognize only the extremes of hormone production – either “very low” or “very high”. Medical reference ranges are purely statistical ranges. By definition, 2.5% of people are below and 2.5% above are above the range.
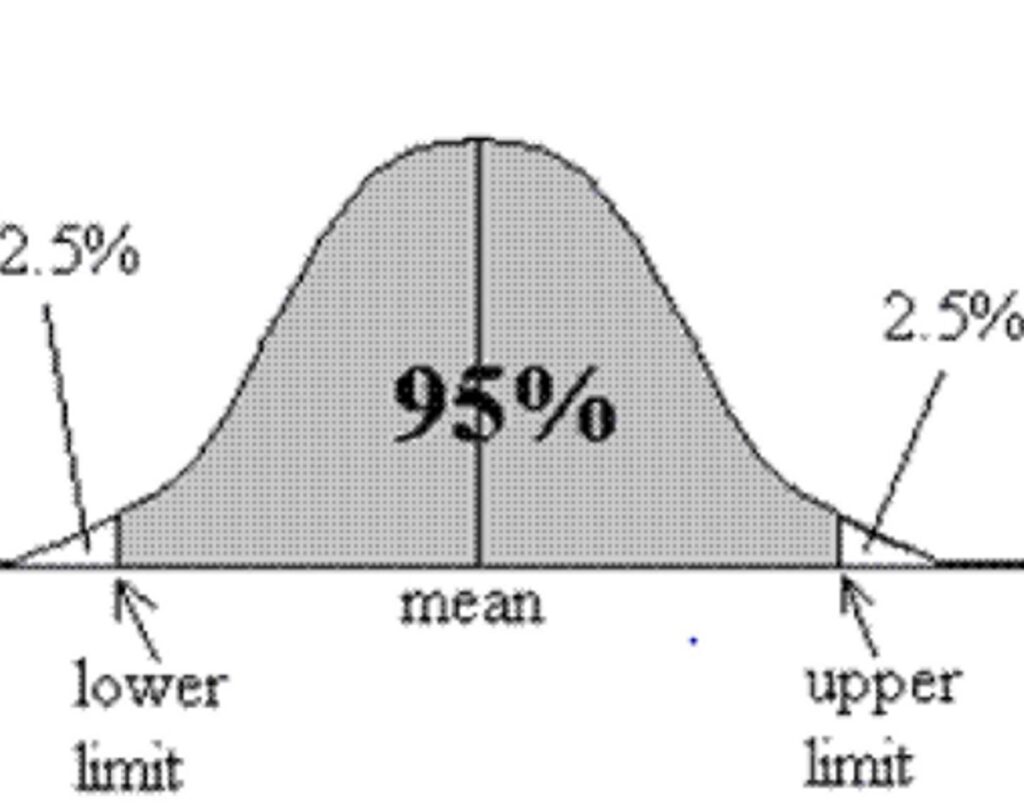
This is an issue because a lot of people who could potentially benefit from hormone replacement therapy fall into the somewhat arbitrary “perfectly normal” range, which is not necessarily the “optimal” range.
In my experience, when doctors look at my blood work, they usually treat it as an “all-or-nothing” issue. If I fall anywhere within the “normal” range, a doctor will tell me everything is great. However, if I am just slightly above or below an arbitrary number, they will tell me something is wrong.
I guess that many people who seek out doctors for problems with hormone deficiencies at their root cause do not fall below the medical reference range and thus often fly under the radar of the current medical system that just looks at values that are flagged. Their values come back “normal”. However, normal for someone 30 years their senior.
For example, the reference range of free thyroid hormones spans a range of factor three. Someone with three times as much thyroid hormone in their body will quite likely feel and function differently compared to someone with only one-third as much – despite both being considered “normal” by the conventional sick-care system.
Hormone crosstalk
The endocrine system is an intricate system. Turn one gear and many others are set in motion as well.
When one of the major hormones is modified, there are many multi-layered second and third-order effects on many other hormones. Interactions occur on many levels, including the hypothalamus & pituitary gland, other endocrine glands, the level of hepatic binding proteins, and ultimately the level of gene expression.
For example:
Thyroid hormones, IGF-1, and growth hormone are all known to stimulate other hormone axes – both at the level of the hypothalamus and pituitary gland as well as at the level of the endocrine gland. Furthermore, thyroid hormones and IGF-1 stimulate cellular activity and therefore they tend to increase the “sensitivity” of target cells to the effects of other hormones. Thyroid hormones stimulate the synthesis of binding proteins (e.g., SHBG) whereas growth hormone and IGF-1 decrease them, which may result in small changes in free hormone levels. Thyroid hormones affect aromatase activity and therefore modulate estradiol levels. Growth hormone stimulates IGF-1 synthesis, which then stimulates an enzyme called deiodinase II (which increases conversion of T4 to T3), and an enzyme called hydroxysteroid dehydrogenase type II, which inactivates cortisol to cortisone.
Analogous interactions are known for other major hormones.
These effects are just the tip of the iceberg as each of the major hormones affects hundreds of genes, and many of the molecular effects have only been roughly elucidated.
Do hormones produce “tolerance”?
The introduction of exogenous hormones is always accompanied by (some) endogenous suppression, which, however, is not the same as tolerance.
Many hormones act on gene expression, either because they act on nuclear receptors (e.g., sex steroids, thyroid hormones) or powerful cytokine receptors directly linked to transcription factors (e.g., leptin, EPO, growth hormone).
Compared to stuff that acts on G-protein-coupled receptors (the targets of most neuropharmaceuticals or recreational drugs), there is much less tolerance to these direct changes in gene expression, which is the most downstream level possible.
However, there will be some tolerance to some effects on neurotransmitter systems (which is what many people are after). For example, after starting testosterone, many experience energy, motivation, and even slight euphoria. These effects are mostly due to testosterone affecting neurotransmitter systems, particularly the dopaminergic system.
Unfortunately, changes in neurotransmitter systems and the ensuing “honeymoon period” are somewhat short-lived. After raising the dose, individuals will often “feel” much better for a short period of time (usually on the order of weeks). However, after a couple of weeks, the brain-based hedonic treadmill takes over and neurotransmitter signaling drifts back toward baseline.
Unfortunately, “how we feel” is not the best guiding factor to determine hormone dosages. “How we feel” depends entirely on the nervous system and we do not “feel” whether the liver, heart, kidney, immune system, etc. are in a hypo- or hyperhormonal state. Therefore, hormones should not be dosed solely depending on “how one feels”.
Hormone tunnel vision
If hormone levels are low, then replacing the hormone in question in a balanced way is a safe, causal, and effective way to rectify the symptoms associated with hormone deficiency. However, it seems that many people are chasing symptoms (e.g., libido, energy levels) and end up replacing hormones in supra-physiological doses even though the putative hormone deficiency was not the root cause of their symptoms in the first place.
For example, guy X might be somewhere around the 40th-50th percentile of testosterone levels. He believes he has every low-T symptom under the sun including fatigue, difficulty losing weight, poor self-confidence, low libido, etc. He is dead certain that his low testosterone levels are at fault for his symptoms and self-diagnoses with “low T”.
Guy X starts to replace his testosterone. Dopamine levels rise and he feels great for a couple of weeks. He believes that he has found the root cause. But as his dopaminergic system adapts, he is soon back to square one. Now the raise, raise, raise period begins, during which he always feels good for some time after every raise, assuming he has simply not raised his dosage enough, even though his levels of testosterone are far above the normal range already.
Gradually he starts to feel “like shit” again. Now he starts to blame the rising estrogen levels. He titrates back and forth testosterone and aromatase inhibitors, assuming he simply has not found the holy balance yet.
However, testosterone was never his issue to begin with and the initial ‘Low T’ problems come back after the honeymoon period. The issues are often complex processes in the nervous system, which might be unrelated to hormone levels. Quite often, the root cause is undiagnosed low-level dysthymia or depression (which is not the same as “suffering”).
If one’s issue is primarily of neurotransmitter or central origin, replacing hormones can definitely bring about (temporary) improvement, particularly replacing hormones in supraphysiological doses in order for them to have supraphysiological effects on various neurotransmitter systems.
Nonetheless, in these cases, hormone replacement is not addressing the root cause and improvement will be incomplete and temporary, even though people can often feel much better over a short period of time.
Abusing hormones for symptom relief is not just unhealthy, but can be quite dangerous and cause irreversible changes in a number of organ systems. Furthermore, it is trading in short-term vitality for long-term health.
Unfortunately, the symptoms of hormone deficiencies overlap with the symptoms of low-level depression and other conditions that are only weakly related to the endocrine system.
In fact, many people with symptoms of hormone deficiencies (e.g., fatigue, low energy, bad sleep, anhedonia,) do have low-normal hormone levels. Some people choose to replace hormones, only to find that it does not bring lasting relief. The meteoric rise in TRT is just one example.
In my opinion, many people would be much better off in terms of safety, health, efficacy, and reversibility if they made major changes to their lifestyle or interfered with neurotransmission directly. For example, I know of two people who switched from testosterone replacement therapy to bupropion, with better and more sustained effects on energy, mood, motivation, and sex drive – the reason why they sought testosterone replacement therapy in the first place. Furthermore, bupropion is leaving most organ systems untouched that would be adversely affected by testosterone.
In sum, some people fare better with antidepressants. As always, the drug regimen of choice is best found through cautious empirical self-investigation.
Hormones can be replaced for life without adverse effects, if they are replaced well.
Recently, I saw a patient who was 81 years old and she was taking 150mcg of thyroxine (T4). She had been on this dose for over 30 years because of total thyroidectomy. Her TSH is completely suppressed and had been this way for decades. She felt “phenomenal” (actual quote), was quite lively, did not need blood pressure or lipid-lowering medication (perhaps due to her higher levels of thyroid hormones) and was definitely healthier than most other 80-year-old patients.
Similarly, I recently had a patient who had a six-pack at 75 years of age. He was type I diabetic and had been replacing his insulin since he was 14, meaning that for 60 years he had been relying entirely on exogenous hormone replacement to survive. Other than the insulin and pantoprazole, he did not use any other medication. He was quite vital, had a full head of hair, and exercises every day. Compared to most other Type I diabetics, he uses only very low doses of a basal insulin (20IU per day) and primarily uses walking and exercise as his primary method of controlling postprandial glucose excursions.
The point I am making is not that these people may have gained an advantage because of their exogenous hormone replacement (which may or may not be true) but rather that, given that hormones are replaced well, one can replace them for life without obvious adverse effects – such as these two individuals, who were relying to 100% on exogenous thyroid hormones and insulin respectively for multiple decades.
Many people I meet are of the opinion, that exogenous hormone replacement must be bad because it is “artificial” and “natural” is better. However, our human bias for preferring “natural” leads us astray, at least in this instance. The artificiality of intervention does not per se lead to “you will eventually pay for your sins” – only if you replace hormones.
Why I do not use peptides
I discuss my personal experience with peptides and why I am literally scared of using them in more detail here.
Hormones & longevity
Hormones and their effects on longevity are discussed here.
How I Biohack My Vitality
This article is a subsection of How I Biohack My Vitality.
Disclaimer
The content available on this website is based on the author’s individual research, opinions, and personal experiences. It is intended solely for informational and entertainment purposes and does not constitute medical advice. The author does not endorse the use of supplements, pharmaceutical drugs, or hormones without the direct oversight of a qualified physician. People should never disregard professional medical advice or delay in seeking it because of something they have read on the internet.
