Each week, I share two observations in my newsletter. These span a variety of topics ranging from recent self-experiments, changes to my protocol, neuropharmacology tidbits, longevity stuff, hormone replacement, case reports, thoughts about medicine, etc.
Entries are posted in chronological order, starting today and ending February 2024 – so from newest to oldest. Every couple of months I will update this post. If you want to get similar observations delivered directly to your inbox, sign up for my newsletter.
Subscribe to the Desmolysium newsletter and get access to three exclusive articles!
My passion project
Some have asked me, why I created Desmolysium. There are no ads, no sales, no promotion of any sort (other than anonymous self-promotion perhaps). After starting his first company, my brother once said that “creating makes happy”. Similarly, Desmolysium is my passion project!
I am officially a cyborg now!
In February, I dislocated my left shoulder during ice skating. The MRI showed that my anterior labrum was torn and I had a SLAP III tear. Ouch. Even though it was my first dislocation and I never had shoulder problems before, I opted for surgery because data on long-term follow-up seems to favor surgery over conservative treatment, particularly in relation to joint osteoarthritis. If the shoulder is not surgically stabilized, it often remains “wobbly” and the unnatural joint movement induces the development of osteoarthritis.
I needed 3 anchors to fix my anterior labrum and part of my superior labrum (from 11 to 1 o´clock) had to be excised because it was completely ripped off the glenoid.
Even though most patients are instructed to wear a sling for 4-6 weeks after surgery, I only wore a sling for 1 week, and thereafter I carefully started to use my arm for light everyday activities (obviously, no abduction or external rotation). After 4 weeks (when most people start active mobilization), I started strengthening exercises most people do not start until week 8.
On Reddit, the fastest recovery I have found was someone who did 10 pull-ups 12 weeks after surgery. I did 20 pull-ups (strict; chest to bar; going all the way down) after 10 weeks. Though I hear that professional athletes are even faster.
While this may seem like bragging (and it surely is because I am proud of my swift recovery!), there is an important lesson to be found.
Sure, for the first month after surgery, I injected teriparatide (a PTH analog with osteo- and chrondroregenerative properties) and a low dose of recombinant human growth hormone (1 IU per day), which presumably helped with soft tissue recovery and osteochondral integration of the suture anchors (I am officially a cyborg now!).

However, the main reason my recovery is going so smoothly and quickly presumably comes down to my short period of immobilization. Immobilization is known to lead to adverse changes in gene expression profiles in osteocytes (bone), chondrocytes (cartilage), and myocytes (muscle) already after 24 hours.
Immobilization is absolutely devastating to the immobilized structure (and the whole body!). I see this daily in the hospital. 80-year-olds lie around for 2 weeks, lose most of their muscle mass, and sometimes remain crippled for life because of that! Many times doctors are overly conservative with when they allow mobilization.
Doctors often do not do what is best for the patient overall but rather what is best for themselves, which is first and foremost not getting sued! This means that if 90% of people would be fine with 2 weeks of immobilization (in fact, would fare much better) but 10% would reinjure themselves, they would have 100% of patients immobilized for 4 weeks, even though this were harmful to 90% of patients. Said in other words, instructions around immobilization are much stricter than what doctors would use for themselves.
I am not saying that this calculation is bad – in fact, if I were a shoulder surgeon I would obviously not want to operate a second time on 10% of my patients within the first month after surgery! Furthermore, I would not want to get sued potentially dozens of times per year because of “negligent” instructions. However, as a patient, my calculation is different.
As with everything in life, forgoing much of the immobilization is a tradeoff. I am trading the degenerative changes associated with prolonged immobilization for a small risk of damaging the anatomical repair – a calculated risk I was willing to take.
What I’d take: my drug preferences for common health problems
(Obviously, lifestyle interventions are important as well but they are not the purpose of this section.)
Hypertension: If I were to choose a drug for hypertension, I would choose telmisartan over other antihypertensives. Telmisartan is an angiotensin receptor blocker (ARB). It has a long half-life and beneficial effects on metabolic health because of its off-target effects on PPAR-delta (a transcription factor involved in fatty acid metabolism). PPAR-delta modulators are banned by WADA because of their effects on endurance capacity. Unfortunately, most doctors choose ramipril or valsartan as their first-line antihypertensive – mostly because of historical reasons.
Dyslipidemia: If my ApoB levels were an issue, I would not even bother with lifestyle interventions (which do not do much for lipids anyway) but would immediately jump to 2.5mg of rosuvastatin (half of the lowest clinical dose) plus 10mg of ezetimibe. Ezetimibe blocks cholesterol reabsorption and is mostly without side effects. Rosuvastatin is a statin (blocking HMG-CoA-Reductase – one of the key enzymes in the synthesis of cholesterol) and at low doses it is mostly liver-targeted. Furthermore, it is very hydrophilic compared to other statins and the lack of lipophilicity keeps it mostly outside the blood brain barrier. Furthermore, 2.5mg of rosuvastatin is known to knock down ApoB levels by about 39%. 40mg of the drug only achieves about 55% despite being 16x the dosage (and therefore carries more non-hepatic systemic effects). Unfortunately, in the hospital I see 40mg of rosuvastatin given out all the time. A friend who is statin-intolerant, has capsules containing 1mg of rosuvastatin compounded for himself, which he can take without side effects (for reference: the lowest clinical dose is usually 5mg). Alternatively, for statin-intolerant people, bempedoic acid is an amazing drug, though unfortunately quite expensive and/or hard to get approved for.
Infections: Obviously, antibiotics are a huge spectrum and the “one-size-fits-all” antibiotics are broad-spectrum antibiotics (which is not good as they kill off most of the healthy flora). For most uncomplicated infections I think macrolide antibiotics are a great choice, particularly roxithromycin. Roxithromycin is dubbed “the doctor’s antibiotic” for a reason. It has a long half-life and needs to be taken only once daily. It targets intracellular bacteria as well (e.g., mycoplasma). Furthermore, it also kills senescent fibroblast and is, after dasatinib, perhaps one of the most powerful clinically available senolytic drugs. Furthermore, unlike penicillin and cephalosporine antibiotics, it is relatively narrow-spectrum and does not wreak havoc on the gut flora. Doxycycline is also a great choice, as is minocycline, which has the additional advantage of inhibiting microglia, therefore helping with neuroinflammation (and potentially Long-COVID). Both are relatively easy on the gut microbiome. Furthermore, both antibiotics also kill off potential unrecognized co-inhabitants that for most people go unnoticed (such as symptom-free infections with intracellular parasites). For fungal infections (e.g., yeast), first-line therapy is usually fluconazole. I prefer itraconazole over fluconazole because itraconazole does not penetrate well into the CNS because it is a substrate of p-glycoprotein. I prefer not to expose my brain to these kinds of drugs unless necessary.
Diabetes: In my opinion, first-line drugs should be GLP-1 agonists, as they go to the core issue of diabetes. Firstly, they lead to weight loss and the loss of visceral adipose tissue increases insulin sensitivity. Secondly, they change insulin levels through acting on the hypothalamus (more specifically POMC/CART neurons), which has drastic effects on blood sugar levels through direct vagal control of the pancreas, liver, and other tissues. SGLT-2 inhibitors are amazing drugs also. However, unlike GLP-1 agonists, they do not address the core of insulin resistance (visceral fat; faulty brain circuits) and are therefore inferior to GLP-1 agonists. I discuss my experience with semaglutide in more detail here. Antidiabetics can also be used by “normal” people as metabolic enhancers – and there is quite some data that these drugs improve general health on many fronts (e.g., rates of atherosclerosis, cancer, or dementia decrease). I will post an in-depth article on my experience with metabolic drugs in the near future.
Hypnotics: Firstly, hypnotics should not be taken daily and the primary treatment of insomnia should be behavioral (How I Biohack My Sleep). But for occasional insomnia (whether it be issues with falling asleep vs. sleep maintenance) many doctors love to prescribe zolpidem, which, in my opinion, is a crappy molecule for a variety of reasons. A much better option, in my opinion, is eszopiclone. Both are Z-drugs but they “feel” very differently (and also produce quite different effects in EEGs). In my experience and the experience of some friends, (es)zopiclone produces a restful sleep with no hangover whereas zolpidem kills my Oura data and is known to lead to all kinds of sleep-walking behavior. In fact, during my night shift two days ago, I had to send an older woman to a CT scan during the middle of the night because she fell out of bed hitting her head after having been given zolpidem by a colleague (even though it is common knowledge that zolpidem should never be given to old people!!). I discuss my experiences with a variety of hypnotics in more detail here.
Choose the newest drug!
As a rule of thumb, the most recently released drug of a certain class is the best one because in order to be approved by regulatory agencies it needs to be superior to the gold standard (under certain circumstances). Superiority can encompass many things such as selectivity, efficacy, toxicity, or side effects. For example:
- Rosuvastatin (the newest statin) is “better” than other statins. PCSK9-inhibitors and inclisiran (injectable siRNA) are both newer than statins and also superior to them in terms of efficacy and also in terms of side effects. The soon-to-be-approved CETP-inhibitors will perhaps be even better.
- Telmisartan, the newest ARB, is better than other ARBs (newer), which are better than ACE inhibitors (older).
- Tirzepatide (2021) is superior to semaglutide (2016), which is superior to liraglutide (2013).
- Roxithromycin (newest) is superior to azithromycin, which is superior to erythromycin (oldest).
- Minocycline (newer) is superior to doxycycline (older).
- Rasagiline (newer) is superior to selegiline (older) – at least in terms of long-term risks.
- Spironolactone (oldest) is inferior to epleronone (newer), which is inferior to finerenone (newest). Even though drug prices are not majorly different for these three drugs (in relation to the tens of thousands of Euros a single patient stay costs), in the hospital I work at, 95% of all doctors use spironolactone, 5% use epleronone, and I have never seen anyone use finerenone – in fact, pretty much no doctor has even heard of it. Many doctors just keep doing what they have been doing in the past, which is something that pisses me off.
- Lisdexamphetamine (newer) is generally superior to amphetamine (older).
- Etc.
There are exceptions to this rule but generally, I find that it holds.
Microdosing finasteride to age more gracefully
David Sinclair looks very young for his age. The guy is 54 but looks like 40. Many people (and even he himself) “claim” that this is due to his intake of resveratrol and NAD-concoctions and intermittent fasting. Bullshit. The guy has been taken finasteride for decades, which is probably the primary reason behind him aging so gracefully.
A friend of mine who noticed incipient alopecia with 25 has been on finasteride (0.25mg) for about 15 years. He is now 42 but looks about a decade younger than he is.
Ashton Kutcher also aged incredibly well in his 30s – presumably/partly due to him taking dutasteride for hair loss. After coming off, he seems to have aged quite a bit.
Similarly, people with long-standing hypogonadism often look much younger than they are. Conversely, people on TRT seem to age incredibly fast – and fat redistribution may not be the whole story. They may look good for one or a few years, but the peak is short-lived.
DHT not only drives hair scalp hair loss, but it leads to accelerated skin aging due to a number of mechanisms which ultimately come down to widespread changes in gene expression. These effects include maturation of hair follicles, pore size and sebum production, and elastin breakdown.
Next to body composition, the skin and its appendages (e.g., hair) are the primary things we can see of another person and therefore are our predominant guide to judging someone’s age.
As a simplification, estrogens (particularly estradiol) keep the skin firm, elastic, and youthful, whereas androgens (particularly dihydrotestosterone) do the opposite.
Back in November/December, I was on TRT. During this time, I noticed small hairs growing in my biceps area. I am quite a non-hairy person and the excess virilization worried me. I jumped on a microdose of finasteride (0.05mg per day – so 1/20th of the recommended dose for hair loss) and the hair growth caused by TRT mostly reversed over a 3-4 month period. This was fascinating to see. I tested my blood levels of DHT and at this dose, my DHT levels were at around 400 (range: 300-800).
In terms of side effects, for the first two weeks my erections were weak and my nipples puffy. This worried me but I am glad I stuck with it. Thereafter, no (noticeable) side effects for me. Libido and erections are as good as ever.
Initially, I also felt and behaved subtly “less manly” but I am not sure how much of that was in my head. Anyway, changing neurosteroids and DHT levels surely has at the very least a subtle effect on my neurocognitive and emotional functioning but hard to say how large that effect is. So, I think that it was not exclusively in my head. Nonetheless, I am also on a TRT lite protocol, which balances out my androgen levels (usually slightly over 1000ng/dl).
All the fear-mongering around post-finasteride syndrome did indeed scare me. However, I figured that in case of worrying side effects I could just taper off (cold-turkey withdrawal is associated with PFS). Furthermore, a dosage of 0.05mg per day is unlikely to cause permanent issues (I may be wrong in this regard).
Given the effects of DHT on the visual aspects of aging, from now on, I plan on using a microdose of finasteride to age more gracefully.
The small reduction in dopamine levels due to AR being highly expressed in the ventral tegmental area can be managed with ultra-low doses of rasagiline.
This is an experiment I am currently running and just as with other experiments, the outcome is uncertain. As of now, I have been on a microdose of finasteride for 4 months and things look good. However, it could very well be that I´ll stop using the finasteride at some point.
The thing I am mostly scared about is a potential flare-up of pubertal gynecomastia – which I am monitoring closely (with some raloxifene on hand). On a genetic level, estrogen and androgen receptors have somewhat opposing effects in some tissues. The reduction in DHT tilts the balance between androgens and estrogens towards estrogen signaling, thus causing gynecomastia in some people.
Just as with everything else in life, there are tradeoffs. In this case, I am reducing some of my “manliness” (though probably subtly) in favor of better skin aging, not developing excessive amounts of body hair, preventing hair loss (which I currently have no signs of), and a reduction in my risk for prostate cancer (my dad had a total prostatectomy last year).
In-depth article here: My Experience With Low-Dose Finasteride to Lock In My Prime
Choose propofol!
In February I had shoulder surgery because of a torn labrum. Most of the time, anesthesiologists use flurane gases (such as isoflurane) to knock people out because flurane gases are cheap (that is why private anesthesiologists love them so much) and easy to handle.
However, post-surgery, most people feel horrendous and nauseous. More worryingly, flurane gases are neurotoxic. There are a couple of publications trying to draw a connection between flurane drug exposure and dementia – with some success.
Thus, I asked my anesthesiologist to use propofol instead of the flurane gases (I got this tip from an anesthesiologist I dated back in February). I specifically asked for propofol via TIVA (total intravenous anesthesia). After waking up from “the best sleep I have ever had”, I felt great and 1h later I was already studying in the hospital bed. Furthermore, propofol is much gentler on brain health.

The price and prize of trial & error
Despite not having depression, I have experimented with about a dozen different antidepressants over the past decade. In the same way that some people feel and function better if they drink coffee regularly, I wanted to find something that is of a net benefit to me.
To minimize side effects, for the most part, I have taken antidepressants at subclinical doses (i.e., lower than the lowest prescribed dose).
Similar to other experiments, most of the antidepressants I have tried were ultimately a failure (though I learned my fair share of first-hand neuropharmacology knowledge). I also had my fair share of side effects (e.g., emotional blunting, diarrhea).
Only one of the experiments was a success: Moclobemide taken at a dose of 37.5mg twice per day.
At higher doses, my cognition and emotions are blunted and I feel “nice” all of the time. However, at subclinical doses, my spectrum of emotions is left mostly intact. Furthermore, on it, I have slightly more energy, a slightly better mood, slightly more confidence, and a slightly greater zest for life. It seems that it does indeed make me feel and function better than baseline with close to zero side effects.
I guesstimate that the compound interest of moclobemide-induced changes in my near and distant future may have been worth the many years of self-experimentation with antidepressants.
Obviously, the second and third-order consequences of something can never be predicted. For example, on moclobemide, I am more social and also have less to no fear. The combination could e.g., cause me to be run over by a car, in which case moclobemide not only led to a net detriment but multiplied everything by zero. But given that inaction is also action, not taking moclobemide could also have its own share of Black Swan events.
However, in general, I feel that in my life, prudent self-experimentation has had way more upsides than downsides. In my opinion, the potential downstream benefit of finding something that truly fits is greater than the downsides (e.g., a couple of sleepless nights) and rare risks (e.g., being run over by a car, PSSD) associated with it.
Edit: Six month after writing this I came off moclobemide as I found out that moclobemide reduces my IQ by roughly 10 points. I always felt that my cognition was subtly impaired on it but I never knew by how much.
Phase II drugs I am looking forward to
There are a couple of drugs I am looking forward to. All of them are antibodies and all of them are currently in Phase II. Furthermore, all of them are made by Regeneron.
Mibavademab: An antibody targeted at the leptin receptor, which it allosterically activates (i.e., it activates it without competing with endogenous leptin). I look forward to it because of a couple of reasons. It helps individuals to recover from starvation-induced brain changes (e.g., long-standing hormone issues, long-standing reductions in adrenergic tone). In fact, quite a few people do not seem to recover from past periods of dieting – particularly dieting down to very low body fat levels. Secondly, it allows individuals to keep body fat as low as they want without starvation-related adaptations. Furthermore, leptin is a highly neuroplastic factor and seems to have great potential in preventing dementia and neurodegeneration. Moreover, from a metabolic health perspective, it prevents visceral fat accumulation and positively influences the metabolic profile. I have a personal interest in all of these things and I am eager to try it once it is approved. I discuss my experience with leptin in more detail here.
Trevogrumab: Trevogrumab is a myostatin inhibitor. Myostatin inhibitors disinhibit muscle growth. These drugs may not only transform bodybuilding (and its overreliance on androgens) but may also be of immense help to old individuals with low muscle mass (sarcopenia). Data in primates is promising and canceled 100% of the loss of lean body mass on a GLP-1 agonist.
Garetosmab: Garetosmab is an Activin A inhibitor. Activin A seems to be quite similar to myostatin but more powerful. For example, the combination of semaglutide plus Garetosmab led to a gain of lean body mass of 7% in obese monkeys (vs. only canceling muscle loss with a myostatin inhibitor). There is currently a human study underway to test both drugs in combination with semaglutide in obese patients. I discuss my experience with semaglutide here.
The neglection of evolutionary psychology in psychotherapy
My psychotherapist usually assumes that my behaviors and thoughts are a reaction to early childhood experiences. For example, I am putting a lot of thought and effort into optimizing my looks. I must not have got enough unconditional love from my parents!
While the dataset of early childhood experiences is undoubtedly important for training the software aspects of neural functioning (and perhaps even the “hardware” aspects of cortical wiring), many of our drives and preferences are undoubtedly hard-coded by evolution.
For example, human greed, the importance of admiration from others, our interest in hierarchies, our preoccupation with what others think of us, our strive for power, our tendency to feel envy, our desire for being sexually attractive etc. are not just reactions to adversities at the toddler stage but rather the result of millions of years of primate evolution.

While for most people this may be tritely obvious, it seems that for many psychotherapists it is not! And this also has implications for psychotherapy: If a certain preference is hard-coded, it will likely not change the way it would if the responsible traumatic experiences are processed to death.
Inhibition of IL-11 signalling extends mammalian healthspan and lifespan
Lately, monoclonal antibodies targeting certain proteins have been all the rage. For example, antibodies targeting TNF-alpha have transformed the treatment of a variety of autoimmune diseases for the last 20 years or so. Or dupilumab (Dupixent), an antibody targeting interleukin 13 & 14, has transformed the treatment of atopic dermatitis and asthma.
Last week an exciting paper was published. The authors blocked interleukin 11. Thus far, interleukin 11 has been elusive. It is thought that IL-11 mostly works in a paracrine fashion, meaning that it mostly acts locally on neighboring cells.
When there is inflammation, among thousands of other things, IL-11 is secreted by cells to increase growth and inflammation in nearby cells, thus serving as an “inflammation amplifier” of sorts. This makes sense in the context of injuries or infections.
However, this is detrimental in the context of aging. Due to mitochondrial damage, accumulation of waste products, increased number of senescent cells, CMV and EBV trying to break out in a state of immunosenescence, etc. inflammation increases with aging. In fact, aging is called “inflammaging” for a reason.
The basic idea is that when one blocks IL-11, one decreases inflammatory processes, which are often associated with growth pathways (e.g., mTOR activation, AMPK downregulation, etc.). Therefore, by dampening the inflammation and growth through IL-11 blockade, this should theoretically increase health-span and lifespan.
Lo and behold, in the paper published 10 days ago, lifespan and health span increased in a similar way as they do when rapamycin is administered (by roughly 25%). This finding, if confirmed by other laboratories (such as the Intervention Testing Program), is huge.
I am eagerly awaiting results in genetically heterogenous mice, primates, and ultimately the approval for a human anti-IL-11-antibody (e.g., for fibrotic diseases).
Microdosing semaglutide
I personally know roughly a dozen people who have had success with microdosing semaglutide. Pretty much everyone, my past self included, has used it effectively for getting and staying lean.
Doses were/are usually in the 0.1mg-0.25mg/week range. Also, most people have greater success with dosing at least three times per week, which keeps plasma levels more stable.
In my country, an Ozempic pen containing 4mg of semaglutide roughly costs 150 Euro. With a dosage of 0.1mg per week (equaling 1 click per day), which is the dosage I have used, a single pen lasts for 40 weeks, amounting to roughly 50c per day. Furthermore, I and others find that at these dosages there are no unwanted side effects, other than appetite suppression and perhaps the need to count calories to not go below an unwise minimum.
Thoughts on MTHFR mutations
A large proportion of people (probably around 50-60% in the Western world) has one of two common mutations in the MTHFR gene. MTHFR codes for an enzyme that is involved in the methylation cycle. It is commonly thought that carriers of one of the mutated forms should supplement with methylated versions of B-vitamins. For example, this is the reason I supplement with L-methyl folate.
In my opinion, the importance of these “mutations” is highly exaggerated. Furthermore, given their prevalence, these “mutations” should be considered wild-type versions.
In my opinion, while it may sound cool to claim that one’s depression or ADHD is ultimately caused by a genetic mutation, this most likely does not represent reality. The most worrisome consequence of being a carrier of these kinds of mutations is elevated levels of homocysteine (which wreaks havoc on vascular health).
Life is not about “finding yourself” but rather about creating yourself.
For years, I have been trying to “shape” myself into the person I want to become (with the goal being constantly evolving). For this, I employ many tools & tactics (e.g., meditation, psychotherapy).
However, the most interesting tools are, in my opinion, biological interventions. For example, let’s say I want to become more driven and productive. Given that drive is partly under dopaminergic control (e.g., more driven people have stronger dopamine signaling – on average), by strategically elevating dopamine levels (e.g., via low doses of MAO-B inhibitors, testosterone), I will automatically become more driven –without any other willpower-requiring input.
Conversely, let’s say I want to do the opposite – become less driven and more “chill”. Given that “chillness” is partly under serotonergic control, by elevating my serotonin levels (e.g., via small amounts MAO-A inhibition), I will automatically become a little less driven and more “chill”.
In theory, I can subtly adjust my personality like I can adjust music on a graphic equalizer. With extreme settings, the final output will be radically altered. With less extreme settings, the changes are much more subtle.
This can even go more meta. By manipulating these neurotransmitters, I can meta-manipulate my wanting for progress vs. now in the first place.
Does neuropharmaceutical intervention change my “personality”? Of course! My personality is nothing more than my pattern of feeling, thinking, and acting – which is ultimately due to my experiences/learning, brain wiring, and brain function – all of which will be changed to various extents with biological intervention.
For example, people who decide to drink coffee every day will subtly feel, think, and act differently – i.e., their personality will be changed in subtle (or not so subtle) ways. Given that the brain wires depending on how it is used, exposure to caffeine will over years also change brain wiring to some (subtle) extent.
Anyway, neuropharmaceuticals or hormones are a powerful addition to the more “conventional” tools for personal development.
Obviously, as always, the best protocol is found by cautious empirical self-experimentation.
There is a disconnect between objective tests and phenotype
Peter Attia claims that the MRI of his spine looks disastrous, yet he does not have any symptoms. Similarly, many people have herniated disks, yet are completely symptom-free. Conversely, others have massive pain with even micro-herniations.
Likewise, some people have “Alzheimer’s brains”, yet their cognition seems more or less normal, while others have obvious dementia but seemingly normal-looking brains.
One of my friends has corpus callosum dysgenesis and his brain is alien-like atypical and “weird” as judged from an MRI scan. Yet, he himself is a professionally and socially competent psychiatrist.
Many people with low testosterone levels in their bloodstream show no signs and symptoms of testosterone deficiency. They have decent body hair, libido, energy, and an easy time building muscle. Others, have every lowT symptom under the sun with a free testosterone in the middle of the reference range.
For example, my testosterone of 600ng/dl is not equal to your testosterone of 600ng/dl (regardless of free levels). Me and you could have different polymorphisms of the androgen receptor (AR). Or we could have different AR densities. Or we could have different versions or amounts of 5-alpha reductase (an enzyme that converts testosterone into the more potent DHT). Or we could have different versions of 3-alpha-hydroxysteroid dehydrogenase (an enzyme that converts androgens into less active metabolites). Or we could have different quantities of androgen-induced changes in transcription factors including tissue-specific differences. Or we could have different accessibility to androgen-sensitive genes. And the list goes on.
Do not get me wrong, there is certainly a strong causal connection between objective tests (e.g., lab values, imaging data) and phenotype but I cannot count how many times I have seen examples where this connection does not hold. Objective tests by themselves can be very misleading and they always need to be interpreted with clinical examination.
My current drug protocol (May 2024)
Drugs I take every day
- Allopurinol (150mg): To keep my uric acid levels below 5mg/dl. Article here.
- Finasteride (0.05mg): To age “more gracefully”. In-depth article here: My Experience With Low-Dose Finasteride to Lock In My Prime
- Moclobemide (2x 37.mg): Makes me a slightly happier, a slightly more productive, and a slightly “better” human being. Article here. (Edit 12/2024: stopped due to moclobemide decreasing my IQ)
- Rasagiline (0.025mg): Balances out the moclobemide-mediated increase in serotonin by elevating dopamine levels. Even this nano-dose is quite potent. Article here. The importance of dopamine is discussed here. (Edit 12/2024: stopped due to having stopped moclobemide)
- Metreleptin (1mg): To “repair” damage from a period of undereating in my early twenties. Article here. (Edit 12/2024: Stopped due to finding out that I feel & function & look well at 12-14% body fat. I am quite sure that two years on metreleptin led to favorable long-term adaptations.)
- HCG (100 IU): Basically TRT “lite”. On this dose, my T levels are above 900ng/dl, my E2 is at 35, and I am not even shut down (my LH and FSH are at the bottom of the normal range). In depth-article here: My TRT Lite Protocol
- Nicotine gum: I chew on nicotine gum whenever I am working. Article here. (Edit 12/2024: Reduced my nicotine consumption to 1h per day.)
Drugs I take weekly
- Rapamycin (5mg): While finasteride counteracts the cosmetic aspects of male aging, rapamycin counteracts many aspects of the aging process itself. Article here. (Edit 12/2024: currently on my 3-month long winter break)
Drugs I take occasionally
- Triazolam (0.0625 mg): Whenever I have a hard time falling asleep, I take a very low dose of triazolam sublingually. I do this about once per week or so. Midazolam would be a better choice but as of now I was too lazy to have it imported from another EU country. Article here.
- Valacyclovir (1g): I take 1g of valacyclovir before every date – at least until I see her HSV-2 status. About 2-3 times per week or so. Article here (section “herpes antivirals”).
Recreational drugs I take occasionally
- Psylocibin (500mg-1g): Great to have a month´s worth of psychotherapy in one afternoon. About once per month. Article here.
- 1,4-butandiol: Precursor to GHB. Great replacement for ethanol, which I never to rarely drink. No deleterious effect on sleep and no hangover. About once every other week.
Drugs I am currently experimenting with
- Adrenaline (50-100 mcg): In search of a short-acting stimulant that does not interfere with sleep. Have only taken it twice so far with disappointing results. Extracted from an Epipen. (Edit 12/2024: stopped)
- Yohimbine (1.25-2.5 mg): In search of a short-acting stimulant that does not interfere with sleep. More promising than adrenaline. For more, see the weekly observation “An ode to yohimbine”.
- Bupropion (8mg-37.5mg): Currently experimenting with microdosing bupropion. Article here. (Edit 12/2024: stopped)
Drugs I am interested in
- NSI-189: Will get hold of pharmaceutical grade NSI-189 soon. (Edit 12/2024: promising). For more, see the weekly observation “My experience with NSI-189”.
- Pitolisant (Edit 12/2024: promising). For more, see the weekly observation “Pitolisant – pure wakefulness”.
Drugs I recently stopped taking
- Semaglutide: At the moment, I want to gain a little weight and semaglutide makes this impossible – even if dosed at 0.1mg per week. Article here.
Many of the drugs I take and/or experiment with, are taken at very low doses to “finetune” things that I perceive to be worthy of improvement. Unfortunately, the concept of microdosing pharmaceuticals is quite unheard of.
Edit: My new protocol: What Changed in 2024?
Bye, bye puffy nipples
A couple of months ago I started a microdose of finasteride to slow down my rate of aging from a cosmetic perspective (Background: Individuals with hypogonadism generally look much younger than they are vs. steroid users and even TRT users generally who look much older than they are.)
My starting dose was only 0.05mg taken every other day. As shared in a previous newsletter, initially I had some puffy nipples which went away after about two to three weeks.
The puffy nipples are due to an imbalance between androgens and estrogens and if the major androgen (DHT) declines, estrogen-receptor mediated gene transcription signaling increases. The result can be a growth in breast tissue, both ductile tissue as well as nipple tissue.
After 4 months on this finasteride dose, I recently doubled my dosage to 0.05mg taken every day (instead of every other day). Dosing is done by grinding the finasteride tablets and then mixing the powder with a specific quantity of methylcellulose powder to get capsules of the desired dosage. Lo and behold, after my dosage increased, my nipples got puffy again.
In order to counter the risk of gynecomastia (which is particularly strong at the beginning of a dosage change but decreases considerably as tissues get “used” to the altered hormone levels), I hopped on a low dose of raloxifene (30mg).
However, on SERMs I feel like crap – my energy and mood go through the floor and my emotional tone becomes non-existent, which shows the importance of estradiol in proper male brain function.
After only a couple of days, I stopped the raloxifene and decided to attack my nipples not from the angle of reducing estradiol signaling (as with a SERM) but rather by increasing androgen signaling. Furthermore, I prefer local/topical therapy over systemic exposure.
I would need an androgen that must not aromatize (hence, ideally, a DHT derivative). Pure testosterone gel could make matters worse due to its aromatizable nature and pure DHT can anecdotally lead to rapid gorillafication (i.e., rapid increase in hairness).
Due to my preference for topical therapy, the androgen must be potent (i.e., highly active in the low milligram range).
Given its molecule-per-molecule potency and poor virilizing activity, oxandrolone-based creams are, in theory, an ideal treatment for puffy nipples and gynecomastia prevention. Unfortunately, these creams do not exist (and nobody has tried this out yet).
I took 100mg of oxandrolone (which I had sent in for HLPC testing to confirm identity and purity), ground it up, and homogenized it with 75ml of CeraVe moisturizing cream, yielding a concentration of 1.3mg of oxandrolone per 1 ml of cream. Picture below.

For the past 2 weeks, I had been applying this cream to my nipples, which immediately stopped being puffy. I will continue doing this for a couple of weeks and then slowly phase it out.
A couple of days ago, I have tested my DHT plasma levels (results not yet in). Given that I know my finasteride-treated DHT levels, the test result will tell me whether there is systemic absorption (being a DHT-derivative, oxandrolone will obviously cross-react with a DHT assay).
Even if there is, at a dosage of 1ml per day, the max possible quantity to be absorbed is quite low (max 1.3mg/d) – and given its very favorable androgenic-anabolic ratio I do not mind any absorption. Furthermore, I only plan on using this gel for a month or so.
Thus far, it seems to do exactly what it is intended to do.
Edit: On the blood test result, my DHT levels remained unchanged, indicating no significant systemic absorption.
The dangers of keeping body fat % too low
I recently dated a woman who has had amenorrhea for over 2 years. She also had cold hands and feet and a blood pressure of 105mmHg. Her SHBG was high. She felt tired most of the time.
Endocrinologists did not know what was wrong with her because releasing-hormone tests had shown that her hypothalamus and pituitary function perfectly well if they are stimulated.
She told me that a couple of years ago she had lost about 15kg of fat. Ever since, she maintained this weight through willpower. Why no endocrinologist (one of them a university professor) has picked up on that important detail is beyond me. The role of leptin in hypothalamic amenorrhoea has been well-known for a long time (study).
Similarly, about a decade ago, I dieted down to single-digit body fat levels (4.8% at my lowest point) and stayed around there for about a year (perhaps the biggest mistake I have made in my life). I did this mostly because of vanity reasons. Back then, my energy levels were abysmal and multiple hormonal axes were in the gutter. My mental health was much worse as well.
Weight regain and starting to eat 3000kcal/d have not fully reversed all of the starvation-related adaptations even years after the fact. Supraphysiological doses of “satiety” peptides (insulin; GLP1-agonists; metreleptin) mostly normalized things though only while I was taking them. As soon as I came off, many of the adaptations came back.
Of all the interventions I had tried, leptin administration was by far the most powerful. I discuss my experience with leptin administration in more detail here.
After weight recovery, former patients with anorexia nervosa have all sorts of issues for a long time – even if they recover more than their original fat mass. For example, in one study, baseline noradrenaline levels as well as stimulated noradrenaline levels remained much lower even 4 years after weight recovery.
Similarly, after the biggest loser study, participants had a negative delta in their basal metabolic rate of about 500-600kcal per day (!) despite being back to their original fat mass. The only hormone that was much lower 7 years after the fact was leptin… (study).
It seems, that the brain somehow “remembers” periods of starvation (whether self-induced or otherwise) and that, for many people, these adaptations are quite stubborn and hardly go away in a similar way obesity hardly goes away after a person has become obese. (Of note, GLP-1 agonists only lower body weight/fat setpoint while the treatment is ongoing but as soon as people come off, most of the weight is regained).
How does this “imprinting” happen? There are two possibilities (at least, I cannot think of any other). Firstly, adaptations happen at the level of neural networks (long-term depression or long-term potentiation of existing networks). Secondly, adaptations happen at the cellular level (perhaps sustained alterations in the expression of certain transcription factors in key neuronal populations such as POMC/CART neurons presumably due to gene methylation).
In sum, maintaining body fat much below the fat set point for a long time seems to carry long-term risks. Some regain their weight and recover fully and quickly. Others are not so lucky. I have met quite a few people who did not recover properly – some did not even recover after becoming much fatter than they were.
I am currently writing an in-depth article about this, and what to potentially do about it.
Why I tell my family and friends to avoid most doctors
Despite being an MD myself, I am quite disillusioned with the way modern medicine is practiced. Most doctors are one-track specialists. They might know how to deal with condition X…but mostly from a perspective of the condition and not the holistic perspective of a patient.
For example, a stellar cardiac surgeon might leave the patient bed-bound for much longer than necessary to protect the surgical repair. The 80-year-old patient might lose so much muscle in the process that he will never go back to a normal walking gait (have seen this particular example many times).
Frequently doctors also leave patients lying in the hospital for much longer than necessary because if a patient is discharged too early, that would have legal ramifications. And the longer patients lie around, the more complications there usually are (e.g., infections with antibiotic-resistant pathogens is just one of many examples). It would probably be better to send most of the patients home much earlier even if that means 5% of them will be harmed.
Furthermore, many doctors simply follow what they were taught by their seniors without looking at the medical literature. For this reason, it often takes years for many doctors to catch up to state-of-the-art practices. For example, in the clinic where I work, roughly half of the doctors have not even heard of semaglutide.
Furthermore, many doctors choose treatments primarily to not get sued. For this reason, many doctors would choose different treatments for themselves or their families compared to the treatments they hand out to their patients. The overreliance on SSRIs and the avoidance of hormone therapies by mainstream medicine are just one example.
My thoughts and outlooks strongly depend on my neurobiology
A couple of years ago I experimented with low doses of irreversible MAO-inhibitor. After taking a single low dose of phenelzine, after 3-4 days (the time the molecule takes to work), I felt a minor version of how I felt on MDMA. I suddenly made lofty plans and my outlook on my future was irrationally positive. I was deeply happy and content.
After a couple of days in this state, my neurobiology swung in the opposite direction. As the MAO-blockade wore off (and my neurotransmitter systems had counter-regulated aiming to restore equilibrium), my thoughts and outlook on my future were irrationally negative. Instead of euphoria, I was filled with anxiety and despair.
Out of curiosity, I repeated this experiment a couple of times. It flabbergasted me every single time and telling myself “Just chill, this is biology.” barely helped – even though I knew exactly what was happening neurobiologically.
Similar things happen on MDMA. Normal state -> bliss & euphoria (“I love my life so much!”) -> Suicide Tuesday (“What is the point?”).
I discuss my experience with depression in more detail here.
I want to end this section with a quote by the philosopher David Pearce:
“Today, meanwhile, many people find it hard to get out of bed in the morning. Given the prevalence of chronic dysthymia, anhedonia and low-grade depression in even the “well” population at large, such inertia is scarcely surprising. Why bother to exert oneself if the payoff is so meagre? Depressive and unmotivated people are likely to find life “meaningless”, “absurd”, “futile”. Nihilistic thoughts and angst-ridden mindsets are common. Feelings of inadequacy and failure can haunt the ostensibly successful. And the world is full of walking wounded whose spirit has been crushed. Conversely (and for evolutionary reasons, less commonly), hyperthymic or euphorically hypomanic people tend to find life intensely meaningful. A heightened sense of significance is part of the texture of their lives. If our happiness is taken care of – whether genetically, pharmacologically, or electrosurgically – then the meaning of life seems to take care of itself.”
While I do not necessarily agree with everything (namely, that happiness is just neurobiology), he has a point.
Yohimbine – a valuable short-term stimulant
Lately, I have been experimenting a little bit with yohimbine hydrochloride, which in my country, is available from the pharmacy (prescribed for treating erectile dysfunction).
Yohimbine inhibits alpha-2-adrenergic receptors. These receptors are coupled to the inhibitory cascade of G-protein receptor signaling. Given that these receptors are often located on the presynaptic terminal, this disinhibits the release of noradrenaline.
Therefore, yohimbine elevates noradrenaline levels all over the body in a way that is much more “natural” than molecules blocking the noradrenaline receptor (NET), such as reboxetine or bupropion. I discuss the science of noradrenaline in much more detail here: An Introduction to Neurotransmitters (and How to Modulate Them)
Because higher doses are quite uncomfortable, I only ever take very low doses. I usually take a single dose 1.25mg and sometimes a second dose a few hours after.
The major advantage of yohimbine is its ultra-short half-life of only 30 minutes or so. Therefore, yohimbine can be taken at e.g., 8pm and should be totally out of the system by 11pm. I am a CYP2D6 poor-metabolizer, meaning that, for me, the half life of yohimbine is considerably longer. The only other stimulant that has a comparable half-life is nicotine, which though is not very stimulating and also addictive. Cave: High doses of yohimbine are quite toxic, particularly to the heart, kidneys, and brain, whereas low doses are probably harmless. Same as with pretty much any other stimulant. As always, the dose makes the poison.
Thoughts on orgasm frequency
Over the past couple of months, I have experimented with varying my orgasm frequency.
After not orgasming for about 1 week, I start to feel slightly more energetic and slightly more emotional. After about 2 weeks, things start to get interesting. By this time, I am quite restless (and horny!). I frequently dream about having sex. Music starts to sound better, and I clearly have more “umpfh” in life. Energy level are much higher than normal. This is quite an awesome state to be in.
Unfortunately, by week 3 and later, my sleep deteriorates to the point where I am waking up regularly at 3-4am without being able to get back to sleep. This happens to me even if I take zopiclone or pregabalin the night before. For me, this state of messed up sleep never goes away.
This is similar to abstaining from food, which also causes insomnia for many. Whenever one of the major hypothalamic drives (drive for sleep, sex, food) is not satisfied, a variety of neural system change – among them the HPA-axis, leading to increased levels of cortisol.
My record thus far was 7 weeks (though I had to quit because my productivity was suffering severely). Out of curiosity, I have measured my levels of testosterone and free testosterone at baseline, week 3, and week 6. There was no significant change outside of normal fluctuations.
Whenever I orgasm, all the benefits go away – but so does the insomnia. I usually sleep for 9 hours for a couple of days. And if I orgasm twice within a short period of time (e.g., having sex twice on the same day or two days in a row – I never masturbate and only ever orgasm through sex.), then I feel that the opposite happens. Instead of being energized and “umpfh”-y, I feel depleted and “meh” for a couple of days. (For me, on TRT, the duration is cut down to 1-2 days instead of 3-4.)
I attribute these changes partly to an increase in dopamine transmission, though I am sure many other brain systems change also, probably directionally towards brain states representing hypomania.
For me, the strategy I have been faring well with is having an orgasm roughly once to twice per week. With this frequency, I am always benefitting a little from the semen retention state. Purely from a “I maximize how I feel” perspective, one week to 10 days would be even better, though sex & intimacy is too important for me at this point in life to cut it in half.
If I go for longer than 14 days, I get early morning awakening to the point that sleep deprivation starts to take over, leading to net detrimental effects.
(Edit: In part because I found these effects so interesting, I started experimenting with TRT again, which led to my current “TRT lite” protocol. On it, similar things happen though the time for semen retention changes to happen is roughly cut in half. I.e., after one week of not orgasming I am usually quite restless with a raging libido.)
Thoughts on caffeine tolerance
For me, whenever I drink even small amounts of caffeine (e.g., 1 green tea, 1 coke) for a couple of days in a row, my baseline energy is much lower. I feel great for 1 hour after drinking caffeine, and then I feel slightly worse than baseline. After 1 week, I then need the caffeine to feel “normal”.
I also start to feel much more groggy after waking up. Usually, I wake up with great energy and can start doing things immediately. In a caffeine-adapted state, I wake up feeling groggy.
I do not know whether I am an anomaly, but, for me, caffeine takes much more than it gives, and I have realized the same thing over and over again.
Conversely, in a recent podcast Peter Attia claimed that, despite consuming 200-300mg of caffeine per day, he cannot tell a difference if he does not consume caffeine at all for a day. (Though he also claims that he does not feel “anything” on 200mg of modafinil and therefore “needs” 400mg – so it might just be that his self-awareness is off…or that he is really an anomaly when it comes to stimulants.)
We are all different and there are certain substances that agree with our unique neurobiochemical/genetic/endocrine make-up while others do not agree with us at all. The only way to find this out is through cautious empirical self-investigation. Nonetheless, because many people are “blindly” consuming caffeine, a short-term uncomfortable self-experiment might be worth it – given that this is something that affects how people feel and perform for years to come.
Random notes on psychiatry
- When doctors get depressed, they prefer to call it “burnout” instead.
- Most people assume that everyone who has thoughts of suicide is in a major depressive episode and that the depression is making them “not think clearly”. While this may sometimes be true, this is not always the case. Some people are at rock bottom and they know it. They do not necessarily have to be “mentally sick” for wanting to end their pain.
- Statistical significance does not mean a drug works well, or at all. If we conduct a trial with 100.000 people, almost any minuscule difference will be statistically significant (but not necessarily clinically meaningful).
- Right now, in medicine and wider society alike, the term “depression” has taken on multiple meanings. The neurobiological process of depression (which is associated with a sharp drop in functionality due to a neural “program”) is called depression in the same way as a non-specific chronic state of unhappiness, “I hate my life”-ness, self-loathing, poor self-esteem, and low energy & excitement. People who claim “I’ve been depressed my entire life” usually do not have neurobiological depression but rather are of the latter type. Antidepressants usually do an okay job with the former, but not so much with the latter. Some help for sure, but in many cases only temporary until the hedonic treadmill turns its nasty gears (”The drug stopped working”). Also, clinical trials for antidepressants enroll participants who are currently in depressive episodes, not people who are chronically unhappy.
- Personality is also not as fixed as most personality psychologists and psychiatrists would like to believe.
- There is a dogma that stimulants make people anxious. This is sometimes true but sometimes also not. Esp. in people with clinical ADHD or “fast brains”, stimulants slow people down because they “stabilize” concentration, which decreases mind-racing. Furthermore, the increase in motivation, enthusiasm, and confidence through increased catecholamine signaling can also be quite anxiolytic.
- Many people with bipolar 1 develop a similar “dementia” as psychophrenics do (”residual negative symptoms”), perhaps because the brain was worn out by being in an overclocked amphetamine-like state for long periods of time. (I do believe that amphetamines may lead to similar issues down the line.)
- A comment by a patient that represents the current state of clinical psychiatry quite well: “I was never truly suicidal until I decided to commit myself to getting my mental health together, following all the psychiatrists’ advice, swallowing all the pills. Seroquel. Risperdal. I slept so much and died inside.”
- Antipsychotics switch the disease from agitation & mania to sedation and emptiness, which by themselves are diseases (but they do not bother others as much).
- The current diagnose-and-drug strategy of psychiatry makes people feel more “crazy” than they are. Let’s say a patient comes in complaining of “depression”. 15 minutes of questioning later you tell him “No, you actually suffer from persistent dysthymia, social anxiety disorder, generalized anxiety disorder, ADHD, and have schizoid personality traits. ”
When it comes to neuropharmacology, first principles sometimes do not work.
Many times they do work – but sometimes they do not.
Androgen receptors are heavily expressed in the ventral tegmentum (the source of dopamine for the mesolimbic motivation system). Hence, when someone is given exogenous testosterone, next to countless other effects, a couple of things change that are coupled to dopamine signaling, such as an increase in libido, increased motivation, impulsivity goes up, emotions become deeper, etc.
Conversely, when someone is given finasteride, androgen signaling decreases (as DHT is a more potent androgen receptor agonist compared to T), which also affects dopamine signaling.
I was one of the lucky ones. Other than one week of weak erections and a couple of weeks of puffy nipples, I did not have noticeable adverse effects. However, I am sure that even though I claim not to have noticeable effects, I almost certainly have measurable ones. For example, if someone tallied the number of times I think about sex or the number of times I get angry, it is probably lower on finasteride even though I do not consciously notice it.
Anyway, a couple of months ago, I decided to add a microdose of rasagiline (a selective irreversible MAO-B inhibitor) to counteract the (putative) lowering of dopaminergic tone due to 5aR-inhibition.
I had been considering this for quite some time but I was hesitant because I do have a tic to “click with my ears muscles” (hard to explain – cannot be seen from the outside but, even though benign, it is nonetheless bothersome). Given the involvement of dopamine in automatic behaviors and impulsivity, I feared that rasagiline would make things worse. Weirdly, after a couple of days on rasagiline, I realized that I have not engaged in this tic almost at all and tic frequency has overall been reduced by rasagiline, even though my first principles would have predicted otherwise.
Random notes on psychiatry: part II
- Mirtrazapine is first and foremost a potent antihistamine.
- The label “treatment-resistant depression” is really bad because it fosters hopelessness (“it will never get better”) and helplessness (“there is nothing I can do about it”) and makes patients believe that they have “uncurable” depression – even though in many cases they either have something really bad going on in their life or their last psychiatrist was just incompetent (e.g., trying out an SSRI and then an SNRI if the SSRI did not work).
- Anhedonia also needs to be differentiated from a “schizoid” personality because being low energy & low excitement is just part of the way how some people are naturally, and there’s no way to “reverse” the symptoms because it is their natural personality.
- Industry-sponsored trials contain a sample that is so highly selected that only about 10-20% of psychiatric outpatients (and below 5% of psychiatric inpatients) would meet the selection criteria to participate in the trial.
- Giving out quetiapine as an antidepressant adjunct is ridiculous…and it happens ALL THE DAMN TIME. The only upside is that it is a sleeping pill.
- The people who don’t want to do anything except take pills are usually the patients who have been on 14 different medications and nothing ever seems to work – and if it does, drugs “poop out” quickly. While some people may indeed be neurobiologically screwed beyond repair, many people may not have “chemical imbalances” or “brain diseases” as much as they think but rather have a very shitty life situation. I am all for pills, but only if they actually help me to get up and change my life.
- Bupropion is not worse than other antidepressants when it comes to anxiety!
- Atypical depression does have many similarities with “adrenal fatigue”, for example, both have blunted HPA-axes, chronic low mood, fatigue, sleeping in, laying around all day, overeating, and being overly sensitive. In both cases, patients will feel better if they are given hydrocortisone.
- A lot of people blindly trust their doctors because as medical professionals they should know what’s best but, unfortunately, that is often not the case. In fact, most people trust doctors like they trusted their parents before they realized that quite often their parents were full of shit.
- For whatever reason, sertraline is known to have a particularly high rate of sexual dysfunction (compared to e.g., escitalopram) and also worse diarrhea than other SSIRs, earning it the appropriate nickname “squirtraline.” Other than that, sertraline is a fantastic SSRI because its affinity for the dopamine transporter.
Case report – Semaglutide for binge eating
Two years ago, a friend of mine referred to me one of his female friends with a binge eating disorder. She had been battling binge eating for almost a decade by that point and had been on countless antidepressants, mood stabilizers, and antipsychotics. She had also been to inpatient rehab centers for eating disorders twice.
I suggested she should take semaglutide. Back then, there was very little academic literature on GLP-1 agonists and how effective they are for a variety of conditions. Therefore, none of their doctors had heard about it (it was poorly known back then) and so they did not prescribe it.
I hooked her up with two pens and made the case for why it would help her. She agreed to try it. Our plan was the following: start semaglutide -> stop binging -> build healthy eating habits -> get to a realistic goal weight -> maintain a binge-free life at her realistic goal weight with healthy eating habits for six months -> taper off.
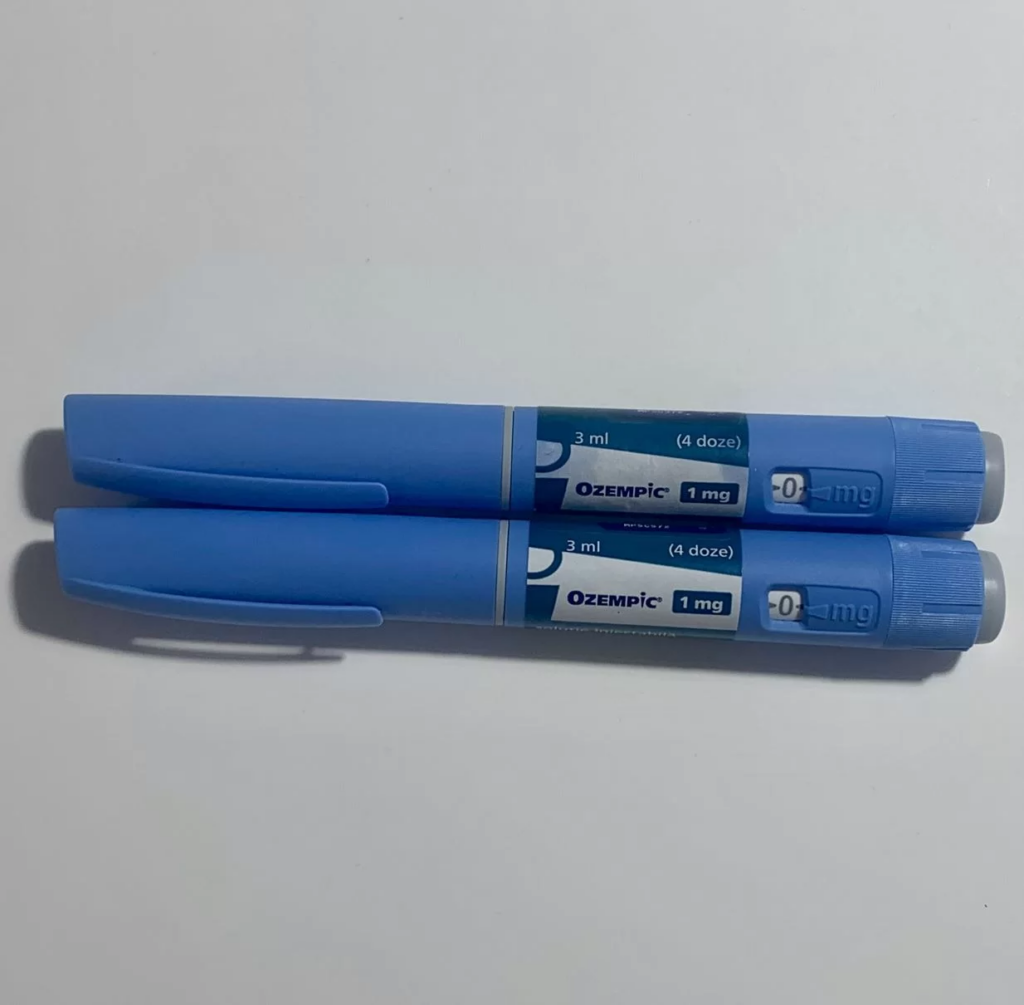
Everything worked out as planned. She had not had one SINGLE binge episode after her first semaglutide dose, which she took for roughly 8 months. She is now one year after having tapered off semaglutide (so 20 months after).
I talked to her yesterday and she is still binge-free and ultra happy about being freed of the chains and shame of BED. She is also about 10kg lighter than before and at a normal BMI. Her eating habits are normal and food has lost the huge role it played in her life. Her fear of certain foods is gone. And she is off psych drugs.
Lesson: Sometimes, “mental” disorders can be treated effectively with metabolic and/or hormonal interventions.
Random notes on psychiatry: part III
- The main benefits of ketamine is a rapid reduction in suicidal ideation – which also serves the hospital/medical system a lot of money.
- Many times, patients claim that “the drug stopped working”. However, it is impossible to peer into alternate dimensions to see what would be happening to the person right now if they were not on the medication. They could e.g., be 30% more depressed and anxious. Also, many times people get so used to their mental state on the medication that they assume it had always been this way.
- The major antidepressant scores in clinical use (MADRS/HADS) have points about “loss of appetite or weight” and “insomnia” but not about “hyperphagia or weight gain” and “hypersomnia”. No wonder that quetiapine and other sedative drugs fare so well whereas stimulants (which lead to a reduction of sleep and a loss of appetite) usually do poorly.
- Antidepressants have a decent efficacy if they are dosed at very low doses (e.g., 2.5mg escitalopram) – which also reduces side effect burden. Unfortunately, most doctors never consider antidepressant doses in the “placebo” range. Furthermore, it also makes no sense to rapidly increase the dosage in every person – firstly, it is not much more effective, secondly side effects increase, and thirdly one cannot anymoe increase the drug when one needs to.
- Psychiatrists prescribe quetiapine like candy… It ruins many people’s lives and health. The major upside is that people stop being a danger to themselves and a burden to others.
- The lifetime prevalence of auditory hallucinations, especially hearing voices, has been estimated to be anywhere between 10-20%.
- When it comes to psych drugs, the response is highly individual. A billion randomized controlled trials and meta-analyses of randomized controlled trials cannot tell you if a medication is, or will be, effective and tolerable on an individual level. This is very different from most non-psychiatric drugs.
- There are some patients that obsess with neuropharmacology: “There has to be some neurotransmitter or brain region that explains why you are the way you are. You just need to dial the right dial and your life will fall into place.” More often than not, this is not the case.
- That vortioxetine does not cause sexual dysfunction is a myth. It definitely does, just less than other SSRIs.
- It is a myth that bupropion should not be given to anxiously depressed patients. From the available data it seems that bupropion does not worsen anxiety (other than in the first week or so) and helps with anxiety almost as much as serotonergic antidepressants.
- Almost everyone on SSRIs will have their sexual function impaired – though many just do not notice it. Vortioxetine is a little less likely than other SSRIs to cause this, though still well above placebo. Antidepressants that are neutral on sexual function are agomelatine, mirtrazapine, reboxetine, and nefazodone. Antidepressants that improve sexual function are moclobemide, selegiline, busprione, and bupropion. Unlike most of the the annoying side effects (diarrhea, anxiety, dry mouth, etc.) sexual dysfunction rarely goes away on its own.
- Opiates have not just wonderful physical-pain-killing properties, but are also excellent emotional painkillers.
- Why would I need therapy if depression is caused by a “brain disease”? Well, etiology and pathophysiology are not the same. I need antidepressants to change neurotransmitters, neurogenesis, and gene expression (pathophysiology), but I need therapy because some things in my mind or life are not the way they should be (etiology). I discuss this in more detail here: What Kind of Antidepressant Should I Choose?
- What most people mean when they talk about depression is a state of long-standing unhappiness with little joy, some anxiety, and just a general state of life dissatisfaction. This is quite different from a “major depressive disorder” as a biological mechanism or entity (characterized by a significant change in their baseline).
The familiarity principle is misleading
Day after day I meet people who are afraid of evil synthetic molecules (pharmaceuticals) but have no problem consuming a dozen or so of glorious natural concoctions (herbal supplements), which are presumed to be good – or at least much less harmful.
Alcohol kills about 4 million people per year and tobacco products kill about 6 million people per year, amounting to about 15% of all deaths. If people who drink and/or smoke would each take three different neuropharmaceuticals instead (let’s say escitalopram, bupropion, and trazodone), their health, brain, loved ones, and society would suffer much less!
While people often do not really bat an eye if you tell them you have a drinking or smoking habit, you get weird looks if you tell them you take three neuropharmaceuticals (“How could you do this to your brain?!”). Similarly, someone taking a truckload of herbal supplements, all of which contain a plethora of alkaloids whose mechanism of action (and long-term safety!) has been poorly identified, rarely gets a second look (especially nowadays as all these influencers promote supplements for financial gain), but the same people would often never take a pharmaceutical drug, whose mechanism of action and long-term safety is often well-known.#
I discuss this in more detail here: Why I Avoid Herbal Supplements
A story about alcohol
I am currently doing my rotation in emergency medicine. I get to see all kinds of weird stuff, including swallowed razorblades, drug-induced psychoses, aortic dissections (only one thus far), anal plugs far up the intestines, and many other things ranging from funny to disturbing.
One of the most disturbing cases I have thus far seen was a 40-year old man who came in with the most gut-wrenching smell imaginable. Turns out he had a 10×5 cm perianal abscess. The abscess was the biggest most of my colleagues (some of whom are working there for 2 decades) had ever seen. The man had been living with the abscess presumably for many weeks, perhaps even months. He told us that he had had it for 4 days only…
After partially bursting spontaneously (that smell!!), it left a second gaping hole in his butt extending all the way to the scrotum. That is when he decided to come to the emergency department. Some of the tissue was necrotic and required proper surgery and the subsequent application of a vacuum system for wound closure.
Before surgery, his wife and his 10-year-old son joined in. His son was wearing big Harry Potter-like glasses, had a small forehead, a short nose, and his mouth was partially open. He was wearing a superhero shirt. He was strolling and staring around the emergency department and he genuinely seemed like someone who has an IQ of 50 or less (for some reason, one just could tell by looking at his dead and gullible eyes).
This was a textbook case of fetal alcohol syndrome. He is about to have a hard life.
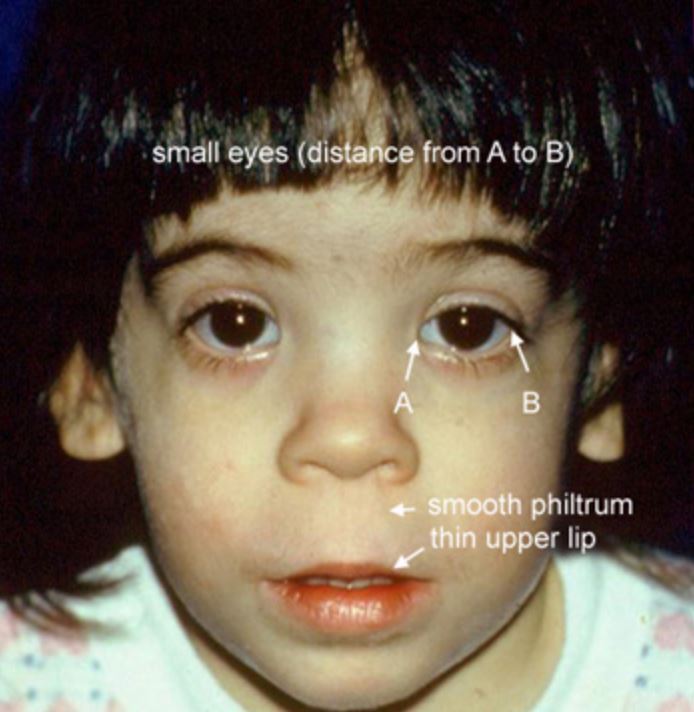
Out of sadness and curiosity I did some research. Fetal alcohol syndrome is the most severe form of prenatal exposure to ethanol. There is a large spectrum of phenotypes, ranging from literally retarded to only slightly impaired in a way nobody can tell. Obviously, the earlier, more often, and heavier the drinking, the more severe the phenotype.
Next to lead poisoning (it is currently estimated that humanity loses about 1 billion IQ points per year because of it!), fetal alcohol syndrome, including its less severe manifestations bordering on normality, may be one of the greatest IQ shredders currently plaguing humanity – let alone the reduction in qualia and quality of life.
In its most severe form (FAS), life expectancy is only 34 years, and 20% of deaths are by suicide. In its many less severe forms, neurocognitive development is slightly impaired (e.g., 5-10 IQ points less than otherwise, more ADHD and autistic features than normal). It seems that roughly 10% of women worldwide consume ethanol during pregnancy, and estimates of people affected range from 1 in 20 (severe cases) to 1 in 7 (light cases).
If the data is correct, this means that roughly 1 in 10 people will be affected by alcohol every day of their life even if they never drink a single sip.
Edit: Following up on last week, the guy with the “abscess” from last week´s newsletter turned out not to have an “abscess” at all but rather a massive necrotizing anorectal carcinoma with metastases in multiple organs. He will probably have a few more months or so to live.
5% happier for 2 minutes per day
For the past month or so, I started doing a very simple 1-minute gratitude exercise whenever I enter a public transport vehicle, which is roughly twice per day.
I close my eyes and start to think of 5 things I am grateful for:
- #1: Something beautiful that happened today (e.g., That I had a great conversation while going for a walk with a friend.)
- #2: Something beautiful that is about to come later today (e.g., Going for my evening run.)
- #3: Something or someone concerning my personal relationships (e.g., That I get along well with my siblings and that I even have them.)
- #4: Something big in my life (e.g., That I am allowed to work in a field that I am intensely interested in.)
- #5: Something beautiful this very moment (e.g., feeling particularly good and rested)
The human brain is a pattern recognition machinery, trained to find patterns for things it is frequently used for. For example, if I train myself to look for people with red hair, it won’t be long before I see red-haired people everywhere. If I frequently play chess, my brain gets better at finding chess patterns.
Similarly, if I frequently think about things I could be grateful for, my brain gets better at “gratitude” simply because the responsible neural networks are trained every day to find “patterns” of things I could be grateful for.
Over time, these thoughts of gratitude came on much more readily – either spontaneously at random times throughout the day or specifically as an antidote to stress, worrying, or grudging. In both cases, these thoughts of gratitude reliably lift my mood and increase my well-being. This small habit of gratitude may be the single best habit I do in terms of effort and payoff.
An ode to yohimbine
Lately, I have been experimenting a little bit with pharmaceutical-grade yohimbine hydrochloride. Yohimbine is an alpha-2 receptor antagonist. Given that a2 adrenergic receptors are located on the presynaptic terminal, the associated Gi-coupled signaling “disinhibits” noradrenergic synapses (the basics of noradrenaline signaling are explained in more detail here). In other words, it disinhpitibits sympathetic tone. As such, it is not just a great fat-loss agent but also a great short-term stimulant.
At low doses, it is subtle and not harsh in any way. On it, I am alert and can think more clearly. There is little to no euphoria (as there is with e.g., caffeine, methylphenidate, or ephedrine). My emotions are more intense and deeper. My libido is definitely stronger. In fact, in my country, the only indication for which yohimbine is approved is erectile dysfunction.
The combination of slightly more alert, slightly better mood, slightly more intense emotions, and not so slightly greater libido is specifically useful before a date. The major downside is that I skew my own perception of her in a positive way – i.e., I think that she is slightly more exciting and attractive than she really is. Similar to what Robert Sapolsky found in his suspension bridge experiments. Short summary: Male participants walked across a suspended/scary bridge. Half of the participants were met halfway by an attractive female. The other half of the participants only encountered the attractive female after crossing the bridge. The people who met the attractive female while in the middle of the bridge rated her as more attractive because of the biological arousal caused by the suspension bridge.
It is currently the only stimulant I use. I only ever use it at low doses and even 1.25mg lasts for a couple of hours, presumably because I am a homozygotic CYP2D6 poor metabolizer, which prolongs yohimbine action. In fact, for me, yohimbine has a half-life on the order of 6-10 hours (instead of the 1-2 hours) because I have 2 copies of “bad” CYP2D6, the enzyme that metabolises yohimbine, which makes yohimbine for me the near-perfect stimulant.
I do not use caffeine because it messes with my sleep. I do not use modafinil because on it I do tasks more thoroughly than intended, which ultimately leads to me wasting a lot of time. Modafinil also makes it very hard to fall asleep, given that the microdose of rasagiline I take potentiates and prolongs its action. I do not use other stimulants such as ephedrine, methylphenidate, or amphetamine because they are too “harsh”, because of the moclobemide, and also because I think that they may be neurotoxic, particularly the amphetamine-class of drugs.
Pitolisant – “pure” wakefulness
For the last two weeks, I have been experimenting with pitolisant, which is perhaps the most interesting neuropharmaceutical I have experimented with in many months. Pitolisant is an antagonist at the H3-receptor.
Simplified, while noradrenaline in the brain is responsible for alertness, hypothalamic histamine is responsible for wakefulness – explained in greater detail here: An Introduction to Neurotransmitters (and How to Manipulate Them)
Histamine in the brain is synthesized by the tuberomammillary nucleus (TMN), which is intricately related and adjacent to the suprachiasmatic nucleus (the “central clock” of the brain). And the major way how the TMN (within the hypothalamus) “wakes up” the brain is via the state of histaminergic tone – highest during wakefulness and lowest during sleep.
It is hypothesized that the wakefulness-promoting effects of modafinil are at least partly due to the indirect increase of TMN histamine release. Relatedly, antihistamine drugs are great hypnotics (e.g., trazodone, quetiapine, mirtazapine, diphenhydramine).
However, for a long time, pharmacologically tapping into the histaminergic system of the brain was off-limits because of the body-wide immunological side effects (particularly mast cell degranulation as it happens during an allergy), which are the reason for the existence of antihistamine drugs such as levocetirizine and desloratadine.
Enter pitolisant. Similar to other neurotransmitters, histamine levels are co-regulated by a negative feedback inhibition at the presynaptic terminal. In the case of histamine, the responsible autoreceptor is the Gi-coupled H3 receptor. By antagonizing this receptor, brain histamine release is disinhibited without unwanted peripheral histamine action.
Pitolisant has been approved for only narcolepsy. Similar to modafinil though, it is a drug that is useful for excessive daytime sleepiness, such as with sleep apnea.
My experience thus far has been quite pleasant. The effect is subtle but definitely present. It seems like consciousness is overclocked by 10-20%. Sensations are more high-definition (similar to the effects of microdosing psychedelics – but without the distortions), I can think better, and I have an easier time being present in the moment. Indirectly, my mood is slightly better because feeling awake just feels good. I am currently on 5mg per day, but I will probably increase to 10mg per day soon.
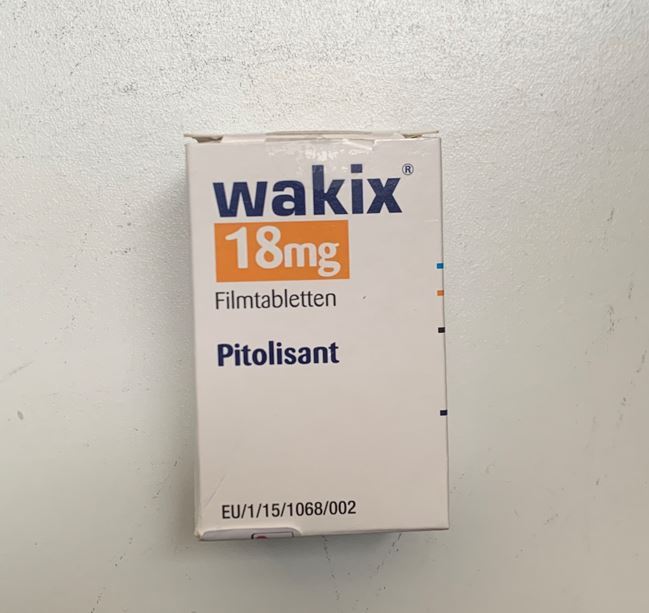
The major and perhaps only downside of pitolisant is its price. In my country, I pay about 10 Euro for a 20mg pill. Given that I am a homozygotic CYP2D6 poor metabolizer, I only need half what other people need for the same effect. So, the increased wakefulness currently costs me about 2.5 Euro per day (5mg), and may soon cost me roughly 5 Euros per day (10mg) should I decide to stay on it, which is a price similar to a Starbucks coffee.
It is mostly devoid of side effects apart from headache, anxiety, and insomnia, all of which though are hardly above placebo levels. Thus far, I have not had a single side effect. I would not be surprised if pitolisant turns out to be a worthwhile dementia prevention tool too given that having an active brain by itself is protective (similarly, depressive states by themselves are neurodegenerative – both directly as well as indirectly through its effect on brain activity and lifestyle).
If I had to put a number on it, I would say that I am roughly 20-30% more awake on it. I expect this to go down to the 10-15% range over time as tolerance builds up. According to the literature, there should be no tolerance build-up but the “scientific” literature claims the same thing for modafinil or eszopiclone… Given that I find life much better if I am thoroughly awake, 5 Euros per day is a small price to pay. I will write a more in-depth article about pitolisant at some point.
The body adapts!
I have been using lip balm before going to bed for roughly two years now. About half of the women I kiss comment on the softness of my lips – I guess partly because of that.
I just came back from a 5-day camping trip with friends. Obviously, I did not bring my lip balm with me and over the course of 4 days, my lips started to get dry and cracked even though I never had this before using lip balm. Presumably, moisture-producing cells in my lips “sense” that moisture levels are already high and stop producing moisturizing secretions whenever I use lip balm. Said mechanism takes a couple of days/weeks to adapt, leading to said effect.
Relatedly, most people are amazed when I tell them that I never use shampoo or warm water to wash my hair, which on the top is roughly 15cm long. I only ever wash my hair with cold water. My hair does not look greasy at all but has a natural shine to it. When I started doing this three years ago, I had greasy hair for roughly 2-3 weeks. After that period, greasiness went down to “normal” levels. Have not used shampoo since.
Similar to my lips, when I wash my hair with shampoo, sebum-producing cells in the scalp sense that sebum levels are lower than they should be, consequently cranking up sebum production (leading to greasy hair after a couple of days of not using shampoo anymore).
Third example. Whenever I wash my hands more frequently with soap (removing endogenously produced oils), my hands start to get sweaty more easily, presumably because moisture/sebum-production is increased.
I find all this fascinating because with each example, there has to be a moisture/sebum-level sensing mechanism somehow turning on an intracellular signaling cascade leading to said effects.
Similar things apply to the central nervous system. For example, in the past, whenever I studied vocabulary, I was soon a much better vocab learner. I expect this to be only partly due to improvements in technique. Presumably, neural circuits related to memorizing vocabulary long-term potentiate. Or whenever I am practicing gratitude, after a couple of weeks, my emotions of gratitude become stronger. In a similar way can a temporary period of fear lead to a full-blown anxiety disorder.
Bones grow in the direction of the pressure applied to them.
People growing up at high altitudes do not just have higher hemoglobin levels, but every level of the organism adapts to the relative hypoxia. From an increased number of oxidative proteins, more abundant mitochondria, and presumably hundreds of other tiny low-oxygen adaptations.
After lots and lots of diving, the spleens of deep divers can “learn” to contract, pumping additional RBCs into the circulation.
Muscles really do grow longer in response to stretching.
Astronauts devoid of gravitational pull develop weird forms of orthostatic dysfunction because their cardiovascular system has adapted to new conditions.
How and that all this evolved is mind-blowing (from a mechanistic level)!
Will I be caries-free forever?
A couple of weeks ago, a friend who visited from San Francisco smuggled something highly illegal into Europe – genetically modified bacteria. A couple of days later, a couple of friends and I were toothbrushing these bacteria into every nook and cranny of our mouths for 10 minutes. Thereafter, we feasted on the most sugary junk we could find to feed our new co-inhabitants.
Streptococcus mutans is the bacterial strain single-handedly responsible for human caries.
BCS3-L1 is a genetically modified strain of Streptococcus mutans designed to combat dental caries. This strain was engineered by deleting the gene responsible for producing lactic acid (the acid component of which erodes enamel) and produces ethanol instead (in minute amounts). Furthermore, it was modified to produce the antibiotic mutacin, which gives it a competitive advantage over native S. mutans because it has been engineered to be mutacin-resistant itself.
There have been some human data for 30 years and nobody was reported to get caries after the first (and only) application. Furthermore, studies in laboratory and rodent models have shown that it is genetically stable, with no apparent side effects, and its ability to colonize effectively suggests long-term prevention after a single application. If things went as planned and my mouth is currently being colonized with it (it will probably take a couple of months for complete outcompetition of native S. mutans), I will never have caries again.
“Significant” does not equal significant!
When I read up on my past shoulder injury to decide on how to proceed, the difference between getting surgery vs. conservative treatment was “insignificant” in terms of redislocation rate in most studies. Only when I looked more thoroughly at the data did it occur to me that there were indeed decent advantages of getting the surgery. Because many times the data sets were quite small (i.e., the statistical power was too low) multiple times the results did barely not reach statistical significance despite a decent effect size.
“The effect was significant”. I read a version of this all the time and I hate it. For example, red meat significantly increases the risk for colon cancer. Even if this were the case (which is debatable), a “significant” (statistically significant) finding does not mean that a finding is significant in real-life (clinically significant).
When most people read the term “significant” they think of it as “having a large effect”. But in science, the meaning of “significance” is different. For example, a difference of 0.1% in toothbrushing frequency will be (statistically) significant if the data set is large enough. Is this finding significant (i.e., relevant) in the real world? No!
Many great methodologists have even suggested that we completely abandon the term statistical significance and just focus on effect sizes (plus the uncertainty about these effect sizes).
What we should care about: Does this make a difference in our lives?. Is it big enough that is worth the cost, the potential harms, the implementation effort, etc.? Unfortunately, whether something is statistically significant (or just “significant” as reported by the media) does tell us very little…
Most scientists are trained to torture their results into statistical significance — to basically use some statistical tests that give them the p-value they need. The reason is simple – to continue to advance their career and continue to be funded, scientists feel the need to prove that they can get significant results. The result is 35 million people who author on roughly 5 million papers every year. Wpihile the results of most of these papers are “significant”, very few of those papers are both valid and useful.
My preliminary experience with NSI-189
I have to dethrone pitolisant as the most interesting neuropharmaceutical I have experimented with in a long time.
Usually, I do not use non-FDA/EMA-approved molecules due to the lack of proper safety data (i.e., Is the molecule safe?) and manufacturing quality control (i.e., Do I get exactly what is on the label?). This includes peptides, bromantane, racetams, and a lot of other molecules that are propagated throughout the quacko-sphere.
However, NSI-189 piqued my interest even though it has not yet been approved.
Whenever I take a low therapeutic dose of ketamine, I feel like a kid for about a week. This is presumably due to ketamine cranking up levels of neuroplasticity.
It has long been known that neurogenesis/neuroplasticity is essential to energy levels, mood, and cognition. Things that induce it (such as psychedelics, traveling, or exercise) have powerful effects on energy, mood, memory and cognition whereas things that reduce it (e.g., aging, loss of environmental enrichment, physical inactivity, hypercortisolemia) are depressogenic.
Hence, it would be interesting to find molecules that induce neurons to grow. To do so, researchers were using a brute-force method (high-throughput screening) to induce hippocampal neurons to grow in vitro. Essentially, they were bombarding thousands of petri dishes with around a dozen thousand different molecules and were selecting the molecules that were inducing the most growth. The lead compound they found would later be modified into NSI-189.
While the exact mechanism has not been elucidated, the most likely explanation is an indirect upregulation of neural growth factors (e.g., GDNF, BDNF, etc.). Screening against a number of enzymes, monoamine receptors and transporters and a host of kinases was negative, and as of yet the exact target has not been found. If TrkB is blocked (TrkB is the receptor for BDNF), most of the effects of NSI-189 seem to be blocked as well.
NSI-189 successfully passed preclinical development (e.g., toxicology) and made it as far as a completed phase II study in humans for depression. Unfortunately, it only worked for a subset of people (as is always the case with depression because depression is a catch-all term for a heterogeneous set of syndromes that do not share the same underlying neurobiology).
It did have an effect on depression but it did not reach statistical significance. However, it reached statistical significance on a number of cognition markers, including memory, working memory, and executive functions.
NSI-189 has been further refined by Chinese research groups into even more potent neural growth stimulators but to my knowledge none of these molecules have human data yet.
Anyway, thanks to being an MD, I have access to proper research chemical sites used by medical universities. For roughly 700 euros I bought 10g of NSI-189. I started it roughly 3 weeks ago, along with a good friend. Dosing is 20mg twice daily. Costs me about 3 Euro per day.
Normally, I do not dream much (or at least I do not remember my dreams). Ever since starting the NSI-189, I have daily vivid dreams. I even started a dream journal. Furthermore, my libido is undeniably higher. Normally, I do not go for second rounds, but ever since starting the NSI-189, I often do and I do not feel depleted after. In the first week, I even had a wet dream one day after having had sex twice, which had never happened to me before.
Maybe I am also subtly more emotional as I am moved to tears more often than normal but it is hard to say conclusively.
My friend also notices the vivid dreams. And he also claims that his memory has gotten better. I personally have not noticed anything on the cognition side.
Anyway, NSI-189 is surely one of the more interesting molecules I have experimented with. The only thing I can say for sure is that it has an effect on my dreaming and libido. I do believe that dreaming & libido are expressions of “brain vitality”, of which neuroplasticity may be a feature.
It will be interesting to see whether the effects on libido and dreaming are sustained. Usually, with neuropharmaceuticals, the effects dampen down with time but given the unique mechanism of action, NSI-189 may be different.
Why I have not built antibodies to metreleptin
Antibodies against therapeutic protein hormones (e.g., insulin, growth hormone, EPO) are usually made by 40-60% of people who take them. Usually, they are without clinical significance. For some reason, antibody development to metreleptin is as high as 95% after only a couple of months on it. Very rarely, these antibodies are neutralizing, meaning that they neutralize metreleptin and also cross-react with endogenous leptin, potentially triggering a temporary condition akin to hypothalamic obesity (i.e., ravenous hunger, rapid weight gain, endocrine dysfunction).
I have been on low doses of metreleptin (to not suffer from the consequences of having little body fat and also to “repair” pathways damaged by years of undereating) for a little over 2 years and I have not made any antibodies against it. How is that?
I took high doses of rapamycin at the start of metreleptin to “teach” my immune system that it is safe (given that rapamycin skews the development of T-cells towards “more tolerant”).
I tested plasma levels of leptin on day 0, day 1, and day 2 to know my baseline and where different leptin doses put me. I then retested 6 and 12 months after that. If I had made ABs against metreleptin than my plasma levels of leptin would be vastly elevated (as they are in every publication to date) because antibodies prevent renal clearance and thus extend plasma residence time artificially increasing plasma leptin levels. Given that my leptin levels are now as high as they were on day 1 (after the same dose), this tells me that I have not made antibodies.
While the exact cause of the very high frequency of development of antibodies against metreleptin is not understood, in my opinion, the primary reason that almost every patient builds antibodies to metreleptin has less to do with metreleptin itself but more with the sheer quantity of protein given subcutaneously. Most therapeutic proteins (e.g., GH, insulin, etc.) are usually given well below 1 mg whereas metreleptin is therapeutically dosed with 5mg (which would be 240 IU insulin equivalent). If you give such a hefty quantity of protein subcutaneously, over time one is going to build antibodies to it due to the “immunogenic” administration whereby a large load of protein is injected into a space where there are lots of resident Langerhans cells.
In sum, I have not made antibodies in over 2 years on metreleptin even though nearly everybody develops them. The reasons I did not are 1) rapamycin (particularly at the start of treatment) to induce a differential differentiation of regulatory T cells and 2) never injecting a big dose at once. Furthermore, if I were to develop neutralizing antibodies (which are super rare), I am quite certain that through my connections I would be able to get hold of mibavademab for compassionate use. Mibavademab is a leptin agonist antibody currently in phase III by Regeneron. There are already individuals who had developed neutralizing ABs to metreleptin being effectively treated with mibavademab.
What everyone should know about oral contraceptives!
In my country, roughly 1/3 of adult women use the contraceptive pill as their primary way of contraception.
As explained in my article on hormones, steroid hormones (e.g., estradiol, progesterone, testosterone, cortisol) affect the deepest level possible: gene expression. If these hormones are altered, on the order of hundreds of genes in every nucleated cell in the body will be altered resulting in profound changes in every tissue.
The primary function of hormonal contraception is the prevention of the LH-peak causing ovulation. This is accomplished by giving sex hormones (in this case, a synthetic form of estrogen and progesterone) exogenously, resulting in the suppression of the reproductive axis. In theory, there is nothing wrong with replacing hormones from the outside – if it is done well. In an earlier newsletter, I argued that if it is done really well, one can have a better (i.e., healthier & more enjoyable) life on exogenous hormones. However, in the case of the contraceptive pill it is not done well at all.
Firstly, the estrogen dosages contained in the pill are insufficient to adequately provide sufficient estrogen receptor agonism to match endogenous levels. Because the pill is given orally, it has a first-pass effect (i.e., goes through the liver first), meaning that there is a disproportionate action on liver cells compared to other cells. This “hyperagonism” in the liver then jacks up clotting factors increasing the risk of blood clots. In order to avoid thromboses, hormone dosages are appropriately reduced leading to appropriate hepatic action but inappropriately low non-hepatic action.
Secondly, ethinyl estradiol (the major form of estradiol used in oral contraceptive agents) does not pass the blood-brain barrier as readily as 17-beta-estradiol (the major form of endogenous estradiol), leading to reduced brain effects. This means that not only are oral contraceptives underdosed (because they have to be!) but the estrogens that are contained also make it into the brain less. It may be partly because of this that users of the contraceptive pill are reported to be more anhedonic and depressed than non-users. In some studies, the odds ratio of depression is around four. A psychologist friend of mine claims that on the pill she could only feel a narrow range of emotions.
Thirdly, because testosterone is a precursor to estradiol but no androgen is provided in oral contraceptives, androgen levels take a major hit. This means that oral contraceptives (inadequately) replace estradiol and progesterone but not androgens, meaning that women on the pill have much lower androgen signaling than normal. While this is desirable for PCOS and acne treatment, this has huge implications for cognition (e.g., women with higher androgen levels are better at mathematical and logical reasoning), emotionality (e.g., drive, libido, “umpfh”), and mate choice, partially because androgen levels affect dopamine signaling.
I find the mate choice aspects particularly interesting. All else being equal, women on the pill (i.e., lower E2 & testosterone signaling) prefer less masculine men. There is a wealth of anecdotal data on women who stop using oral contraceptives in order to conceive only to find out they are no longer attracted to their partners (Attraction is not a choice!!). One wonders, whether this large-scale manipulation of sex hormones also contributed to the rise of boy bands and boyish-looking celebrities.
One of my ex-girlfriends does it better:
- Instead of ethinyl estradiol, she replaces her estrogen with a estrogen gel containing the bioidentical 17-beta-estradiol (normally reserved for postmenopausal women). This prevents the LH-peak just like oral contraceptives do and therefore provides effective contraception. Furthermore, because it is given transdermally (i.e., no first-pass effect) she can reach adequate blood levels of estradiol without increasing her risk for blood clots. Moreover, the 17-b-E2 makes it into the brain like it should (as it is bioidentical). Using this method, she can put her blood E2 levels where she feels best, in a similar way men do with TRT (article about my current use of TRT soon!).
- She uses micronized progesterone instead of synthetic progestins. The bioidentical progesterone metabolizes normally into allopregnanolone, which users of synthetic progestins deprive themselves of. Allopregnanolone is one of the most important neurosteroids in the human brain.
- She also takes a low dose of DHEA, an adrenal androgen, which adequately elevates her testosterone levels into the normal range. Normally, testosterone levels tank if estradiol is administered exogenously due to the HPTA shutdown. DHEA is an effective way for females to elevate androgen levels (though it has little to no effect on males).
Unfortunately and sadly, many gynecologists do not know much of this…
From the outside, you cannot tell.
While working as a psychiatry intern, this has been my key lesson.
Patients include a lot of people for whom everything looks “great” from the outside. They come in and open the baggage they are lugging around day in, day out, completely outside of everyones awareness.
I remember a doctor coming in with a suicide attempt with sulfonyl ureas (because his wife had left him), a PhD student coming in with devastating depression, a lawyer with severe bipolar swings, a young good-looking kindergarten teacher with obsessions about death, another doctor with incredibly violent and gory daydreams. If one had seen these patients in daily life, it would be impossible to tell…and if one had googled them (not that I would ever google patients!), one would think they would lead perfectly pristine lives. Most of us are great at keeping up our façade because we have been conditioned to do so (partially because of evolutionary inclinations to not lose social status).
Dreaming intensity as an indicator of neurogenesis
Kids dream more vividly than adults. I speculate that this may be related to the “amount” of neurogenesis they have. For me, this “dreaming hypothesis” aligns well with educated guesses of what should elevate levels of neurogenesis.
Things that cause more intense dreaming for me:
- NSI-189 – an agent designed to increase neurogenesis. I discussed my preliminary experience with it in an earlier newsletter. I have been taking it now for roughly 6 weeks – dreams are still going strong! Interestingly, on days I do not take it (e.g., because of traveling) I still dream more than I did before.
- Psylocibin. After taking psychedelics, I dream more for a couple of days. Some of my friends report the same.
- Same with ketamine. After a single dose of ketamine, I dream much more for about a week or so, coinciding with what we know about ketamine and how long it affects neurogenesis.
- Starting metreleptin. I dream more readily for 1-2 weeks or so.
- E2 manipulation. Estradiol is hugely important for neural health and a lack thereof may be the main reason why women are twice as likely than men to develop Alzheimer’s dementia.
- Nicotine close to bedtime (which I do not recommend because it gives me a hard time falling asleep and because it reduces my SWS).
- Growth hormone. I have experimented with it a couple of years ago. Whenever I started taking it, it made me dream intensely for a few weeks and then dreams decrease to a lower level (but still above baseline). After starting growth hormone, nearly everyone reports vivid dreams. It may be no coincidence that kids have much more growth hormone secretion than adults. GH receptors are widely distributed throughout the brain, particularly the hippocampus, a brain structure intimately connected to dreaming. Furthermore, growth hormone also has potent effects on the brain through IGF-1. There is also a linear inverse relationship between IGF-1 levels and dementia. An article on growth hormone soon!
In sum, for me, other than experimenting with agents that are known to be neurogenetic (e.g., NSI-189, ketamine, psylocibin), dreaming (and presumably neuroplasticity) has a lot to do with my hormones.
We are all different – doses need to be individualized
One friend of mine is knocked out by 0.3mg eszopiclone, including feeling battered the next day. Another friend barely feels the full 3mg. Even 12.5mg of trazodone cause me to have a hangover whereas some people can take 150mg without issue.
One friend who is on a full dose of tranylcypromine (an irreversible inhibitor of MAO-A and MAO-B) feels quite few psychomimetic effects from 2g of psylocibin even though MAO-inhibitors are known to potentiate the latter. Conversely, I feel quite “well” on just half a gram.
Another friend of mine microdoses bupropion and claims to feel doses as low as 5-8mg. Similarly, when I dose modafinil, I usually only take 15-20mg of it. Conversely, Dr. Peter Attia was supposedly on 400mg of modafinil per day for many years during residency and claims to not feel 200mg when he now takes it. Similarly, a colleague of mine claims to take up to 700mg of modafinil while studying for the USMLE. According to him, he cannot feel a difference on 200mg.
I get jittery and hyper-excitable on just 50mg of caffeine, whereas others barely feel a coffee, even if they are not caffeine-tolerant at all.
I feel quite stimulated on 75mg of moclobemide whereas some others do not feel anything on 150mg.
The main point is that our neurobiochemistry is unique. The best (and only) way to go about finding the “correct” dosage is cautious empirical self-investigation. Too bad, that most drugs come in fixed dosages and that doctors rarely take the time to properly explore proper dosage-finding with their patients. I am confident that many patients stop prescription drugs way too early simply because they were instructed to take dosages that were far too high for their unique biology.
Moclobemide appears to lower my IQ
For a long time, I suspected that moclobemide was making me “content” at the expense of cognitive horsepower. On moclobemide (even very low dosages), my thinking is more shallow, presumably, because I am at cognitive “ease”. I discuss this in more detail here.

As an experiment, I recently weaned off moclobemide. Before coming off, I performed the online Mensa IQ test. After 4-5 weeks, one week after coming off moclobemide, I performed the same test under mostly similar conditions (e.g., time of day). I scored exactly 10 points higher.
While many factors might be at play (e.g., having done a similar test in the past already, energy & mood subtly different on that day, etc.), I do feel that this test result is quite representative of how I feel moclobemide affects my cognition. On it, I sometimes scramble for words and my eloquence is worse. Furthermore, I do not think as deeply about things. I think that the main reason moclobemide messes with my cognitive ability is that it changes my dopamine/serotonin ratio.
Interestingly, my second test result was about the same as I had scored 10 years ago. This means that my decade-long hard-core biohacking (whether it be hormones, rapamycin, antidepressants, or stimulants) has not messed too much with my hardware in terms of neurotoxicity or neurodegeneration.
I have been off the moclobemide now for roughly 6 weeks and I like my “natural” state better. I am more cognitively agile, more emotional, slightly more aggressive, a little more extreme, and more “human”. On moclobemide, I am more “content” in the moment and do not want to spend as much cognitive effort on things. For me, moclobemide is a great pick-me-up agent if I feel depression is looming but it is not a suitable “enhancement” because it may actually make me worse off long-term.
I have been off the moclobemide for a couple of months now and I like my “natural” state better. I am more cognitively agile, more emotional, slightly more aggressive, a little more extreme, and more “human”. On moclobemide, I am more “content” in the moment and do not want to spend as much cognitive effort on things. For me, moclobemide is a great pick-me-up agent if I feel depression is looming but it is not a suitable “enhancement” because it may actually make me worse off long-term.
Overall, I spent roughly 3 years on moclobemide and these 3 years have been among the most productive and most enjoyable years of my life. How much moclobemide had to do with it is hard to say.
Friends do not find that moclobemide affects their cognition and moclobemide is also frequently prescribed for cognitive impairment in the elderly – we are all different!
Nicotine for self-conditioning
For the past couple of years (maybe 5?), I have been using nicotine gums and lozenges while studying or working on cognitively demanding tasks. I noticed that I somehow self-conditioned myself to work & study.
After a 1 month break (no withdrawal whatsoever), I started to introduce nicotine gums for 1 hour per day. During this hour (which I call “systems”), I read over old notes, whether my old science notebooks, my journals, or some Word documents I wrote over the years. I usually have to overcome a mental hurdle to start with this, simply because this hour is cognitively quite demanding. However, occasionally I do stumble on practically implementable gems that make spending one hour per day this way totally worth it.
Since using nicotine in this targeted way, I find that I now look forward to this hour more than before and the mental inertia to start has decreased considerably.
If used selectively, I think that nicotine is a fantastic self-conditioning agent because of the way nicotine works in the brain. Others use coffee for this but I have my qualms with caffeine. I make sure that my nicotine products are flavorless. I do find that any sweetness (whether caloric or non-caloric) does distort/worsen cognition by creating an opioidergic pleasure reaction.
The biggest risk to this is an “expansion” of the tasks/hours one allows oneself the nicotine. I do think that having a brain that is exposed to nicotine 24/7 is a net negativecompared to not being on nicotine at all.
Bryan Johnson – The world’s most expensive eating disorder
When my body fat was ultra low (4.8% at my lowest) I became ultra-obsessive, tolerated unbelievable amount of self-torture to reach my goals (e.g. cold showering despite tissue necroses on multiple toes on both sides of my feet), and I had the weirdest eating habits of anyone I know. I was also super rigid about timing and I could not mentally stand breaking my fasts by even a couple of minutes.
My need for control was very high (just as much because of my eating disorder than the other way around) and I meticulously tried to control my environment. My blood pressure (roughly 105mmHg), resting heart rate (low 40s when sleeping), and body temperature (roughly 35.8-36.5) were all very low. I had a fixed caloric intake (2000-2100kcal/day) and whenever I overshot it, I made sure to balance it out over the next couple of days. My face looked gaunt. My vitality was non-existent.
Just like Bryan, I was never underweight because I had a fair amount of muscle. I had an eating disorder concealed under the veil of “health and fitness”. However, what was really going on was starvation. Nowadays, I quickly recognize it when someone else has an eating disorder, even borderline disordered eating.

When body fat gets to very low levels, for evolutionary reasons, people are set to become obsessive, rigid, and engage in OCD-like behaviors. We also see this in about every mammal we study, and Bryan Johnson is no exception.
Upon starvation, sympathetic nervous system activity falls, leading to low blood pressure (as far as I know, Bryan’s is around 105mmHg systolic) and heart rate (Bryan’s is in the low 40s while sleeping).
Furthermore, because sympathetic nervous system activity gets so low (and levels of noradrenaline are so low), during sleep resting heart rate drops and heart rate variability increases quite a bit. While having a low heart rate and high HRV can be suggestive of restorative sleep, the change in these parameters can also be suggestive of an abysmally low sympathetic activity. Hence, one could argue that he cheats his way to a “great” sleep score by having a pathologically low sympathetic tone.
In anorexia nervosa (and the huge spectrum of pre-AN states), body temperature often falls to 36C – 35.5C, so borderline hypothermia. Bryan just released a newsletter this week “bragging” that his body temperature hovers around 34.8C, which means outright hypothermia. Mammalian enzymes have evolved to function well in a very narrow temperature range and when the temperature is considerably above or below, kinetic equilibria are going to be perturbed.
To quote from his newsletter: “My health program has me metabolically cold plunging. Since starting Blueprint, my body temp has cooled 4°F in 3 yrs, now at 94.8°F. This technically qualifies as minor hypothermia. To put this into context, it takes swimming more than a mile in ice to achieve an equivalent temperature reduction as mine.”
Well done, Bryan.
His carotenemia is also a hallmark sign of being in starvation and nearly every anorexia patient has it. Most people think that he is so pale because he simply avoids the sun. Wrong. His body is so cold and his blood circulation is so centralized that there is little cutaneous blood flow, therefore the red color of hemoglobin does not “shine” through the skin causing his vampire-like color.
Edit: This entry then evolved into this article, The World´s Most Expensive Eating Disorder, which is one of the most read Desmolysium articles.
Positive effects I have noticed from gaining weight and increasing calories
Starting in April, I made it a goal to gain 1kg per month, whether fat, water, or muscle did not matter to me. To do so, I increased my caloric intake to roughly 4000kcal per day. I gained 7kg thus far, I would say roughly half fat and half muscle.
Ever since embarking on this experiment, I have not been sick a single time. Between August and November, I was working in emergency medicine and we had multiple sick waves, during which most of my colleagues got sick at least once. I never wore a mask and interacted with sick patients on a daily basis. I have not gotten sick once.
I feel that I have a genetically pretty robust immune system as I barely ever got sick until I started undereating due to vanity reasons at the beginning of my 20s. It seems that the weight gain + increasing my calories has “restored” my immune function. Before, my caloric intake (roughly 3000kcal) and my body fat levels (roughly 10%) were probably too low for functioning optimally (in terms of vitality). While I have not confirmed my current body fat levels via DEXA, I guesstimate that I am roughly at 12-14%, probably closer to 14% than 12%.
Both insulin and leptin have large effects on the immune system. Furthermore, both hormones also have stimulatory effects on other hormone systems (e.g., thyroid hormones), which then also affect the immune system.
Furthermore, I now also have considerably more energy than before, which is worth a lot to me.
Interestingly, multiple female friends told me that I look better now because my face seems healthier and more vital. One friend also commented my body looks less “freaky”. This goes to show that what most males think is attractive (ripped) is often not in line with what most females think is attractive (quite muscular & quite lean but not too muscular & too lean).
Moreover, from time to time I struggle with anhedonic depression. This happens about 3-5x per year lasting a couple of weeks. During these times, I do all the things I normally do (e.g., work, gym, friends) but I feel quite little. The weird thing is that from the outside nobody can tell. When I tell friends that during these times I actually feel quite a little, they usually do have a hard time believing me because I am just like always. However, on the inside, there is emptiness. It seems that the frequency of these episodes happening has gone down quite a bit over the past six months and only happened once. I think this could be related to the weight gain and the increased caloric intake though I also started taking TRT lite at the same time which is a potential alternative explanation.
My experience with increasing my dopamine levels: upsides & downsides
(Background: Rasagiline is an irreversible MAO-B inhibitor. As such, it inhibits the breakdown of dopamine and trace amines. Rasagiline and selegiline are the only drugs currently available that increase dopamine in a “natural” way – they inhibit breakdown and thus dopamine content of presynaptic vesicles simply becomes larger. It elevates dopamine in a very different way compared to reuptake inhibitors (such as modafinil) or release-inducers (such as amphetamine). It also “feels” quite different. A single dose has subtle effects on the order of weeks due to the slow turnover of MAO-B.)
Whenever I add microdoses of rasagiline to my stack, quite soon (hours) I notice a couple of subtle and not so subtle changes.

During the first couple of days, there is a low-grade euphoria and generally an increased feeling of “I love life” and purpose. However, these go back to baseline after a couple of days, even with continued dosing. This is very similar to the honeymoon phase of testosterone replacement therapy, which is also due to temporary “dopamine supersensitivity”.
Whenever I add rasagiline, I notice that I become more impulsive. I generally try to open WhatsApp only every couple of hours but on rasagiline, I sometimes open it “without even thinking” many times per day. It seems that mindfulness decreases and the gap between “stimulus and response” becomes smaller. This is in line with what we know about dopamine. A friend says, that on rasagiline he procrastinates all day because he is just so impulsive and constantly goes down rabbit holes. (Conversely, another friend claims that on rasagiline he procrastinates less because he finally has the willpower and agency to just commence working.)
Dopamine generally increases the range of activities an animal finds worthwhile pursuing and I definitely notice that. When my dopamine is higher, it seems that I am generally more curious and interested in things.
I also become a little “anti-chill”. I find pleasure in working all the time and relaxing becomes hard and chore-like. I am naturally this way but on rasagiline it becomes too much. I need to be constantly “doing” something.
My ex-girlfriend usually noticed on day one when I started taking even a microdose of rasagiline (She was aware of what I was taking and why – she is a doctor). She is quite perceptive and on rasagiline my behavior is nudged towards a specific direction, which she picked up on without fail. On rasagiline, I am also a little more prone to wanting to have things go “my way”. I am also a tad more of an asshole due to the combination of impulsivity, impatience, and reduced cooperativeness. Rasagiline was definitely not good for my relationship.
My mood seems to subtly improve on it (a lot during the first few weeks, from then on much less but probably still above baseline).
On rasagiline, I also seem to be less prudent (e.g., my threshold for engaging in new experiments becomes much lower).
On it, my thinking is rushed and almost becomes ADHD-like (which is not necessarily bad). I “jump” quite a bit and sometimes in conversations I can make unexpected subject changes, due to my brain becoming “faster”.
On it, I am also slightly more emotional and moved to tears more often.
After experimenting with different dosage ranges, I settled on a very low dose – 0.025mg per day (standard dose is 1mg per day), which means that I take 1 tablet in a span of 40 days. I tried higher doses but that did not go too well. It is always fascinating how powerful rasagiline is. I do think it is more powerful for me than many other people because my dopaminergic tone seems to be quite high already.
If it were not for rasagiline, I may have not started these Weekly Observations (which I started back in February three days after restarting rasagiline after a long hiatus from the molecule). After starting rasagiline, I also wrote a dozen new article drafts within the span of a couple of weeks (none of them have been published on Desmolysium thus far).
I am currently off rasagiline because overall it seems that the risks of the drug (mostly stemming from the increase in impulsivity and decrease in prudence) and the effects it has on my relationships (e.g., less cooperativeness) are not worth the gain in speed. If you want to go fast, go alone. If you want to go far, go together. Rasagiline only helps with going fast but may actually reduce my chances of going far.
However, I am positive that I will use it again (e.g., during work sabbaticals) from time to time in the future, just not as a fixed part of my stack.
Generally, most people assume that having more dopamine is better. Every single person I know that has tried rasagiline has eventually come off it. Some still use it during short periods only. If “more dopamine was better”, I am sure that at least one person would have included it as a fixed part of their regimen. Of note, at these dosages, rasagiline has pretty much no side effects other than the unwanted effects of increased dopamine itself.
What some of my friends noticed:
- More fuzzy thinking; constant thought-jumps
- Increased tendency to procrastinate (some noticed a decreased tendency to procrastinate). On rasagiline, it is much easier to “start doing”…but it is also much easier to give in to impulses, which for some people can have net detrimental effects on productivity.
- Greater agency (e.g., “On rasagiline, I always complete my daily to-do list.”)
- Increased tendency to give in to urges (e.g., nicotine, porn, sweets, buying lottery tickets)
- Increased sense of purpose
- Greater curiosity and creativity
- Wanting to break up with current partner
- More frequent thoughts about sex; increase in libido; urge to be more promiscuous
- Increase in aggressive and violent thoughts
- Being more dominant in social situations
- Being more eloquent
For more on dopamine, read here: The Brutal Neglection of Dopamine
Why I do not use peptides
In my early twenties, I used BCP157, TB500, and CJC-1295 DAC. To make sure that I got what I paid for, I contacted the peptide supplier (one of the most renowned suppliers in the EU at the time) and they sent me their certificates of analysis. At the time, I sprained both of my ankles doing a stupid stunt. I used the BCP157 and the TB500 only on one ankle (superficial subcutaneous injection) and not the other. I have not noticed a difference in their healing rate. The peptides could have been bunk/scam (as everyone can fake a certificate), or they did not work for my particular injury, or tit could be that peptides do not work at all (even if you got exactly the molecule you paid for) and most of the people who claim “amazing results” are just sham-treating themselves.
Most people criticize the FDA for banning the sale of peptides (e.g., BCP-157, Dihexa, MOTS-C, etc.) – “Big pharma is only wanting to make money”. The FDA basically said that peptides need to be studied like other drugs are required to be studied – a perfectly rational and valid reason and this is how it should be. Drugs, particularly if they are injected by people, need to be studied properly because there are more things that can go wrong than the average lay person realizes.
The truth is, few of these peptides have been studied systematically. Yes, there may be a handful of scientific papers on them. However, usually, the papers around a specific peptide come from a single obscure research group, sometimes from Eastern bloc countries.
Having co-authored a few papers myself and being friends with people who made the mistake to go into academia made me realize how untrustworthy many “scientific” papers are – particularly if they have been published by low-quality journals, or worse even, by open-access journals (i.e., just pay money to publish a paper, often without the peer-review process). Many people have long realized that people are incredibly gullible and quite easy to fool, which resulted in publishing scientific papers having become the latest marketing scam.
I do not trust most papers published on peptides and pretty much none have been replicated. I am sure there is a lot of bullshitting going on for profit.
It may very well be that some of these peptides deliver on their promises. However, the truth is, for most of them there is a lack of human exposure data. Furthermore, if one does believe their mechanism of action (I personally do find at least 50% not credible), how do you know you are not also impacting highly regulated biological processes leading to potentially disastrous consequences?
One cannot make the same argument for currently approved drugs. For most approved drugs we know pretty well how they work (with a few exceptions) but we know for close to 100% of them what their side effects are and whether there are rare idiosyncratic reactions. Furthermore, every single drug approved by the FDA or EMA needs to go through very extensive toxicology testing, including generating multi-generational exposure data and histology examinations. For peptides, none of that data has ever been generated. So, for approved drugs, I can do proper research about what can go right and wrong – which cannot be said for peptides.
Sure, occasionally, there was some bullshitting done by big pharma companies (particularly before the 2000s). Also sure, there may be some “statistical lying” going on. But outright fraud is pretty rare, in my opinion.
Moreover, I do not trust the underground manufacturing process, including most compounding pharmacies. There is a host of bodybuilders who use underground lab growth hormone (with impurities and/or amino acid alterations), leading to the build-up of antibodies, some of which are neutralizing. Immunogenicity for protein hormones is a concern and was one of the most commonly cited reasons for the FDA to ban a specific peptide – the concern is 100% valid. If you inject strains of an amino acid (i.e., peptide) the immune system may detect this as “foreign” and generate antibodies. Sometimes these antibodies may crossreact with endogenous proteins.
Furthermore, there is no way for the user to know whether he is getting what he paid for. It is reconstituted white powder that could be a thousand different things. The most common case is probably harmless white powder of nothingness (i.e., no active ingredient – a scam) – and given the human propensity to feel different after sham treatment (particularly after “invasive” injections) people often come back for more.
When I worked in the ER department, quite a few times people came in claiming to be sick. After some time (and with the use of objective tests) you get the hang of who is sick and who is not. Quite a few times, I have seen somebody feeling “a lot” better after an infusion of saline water or vitamin C.
From the examination of supplement companies, we know that a large number of them scam their users. For example, ephedrine pills often contain caffeine instead, 1mg melatonin pills often contain 3mg, and various herbal extracts with artificially scientific sounding names to appeal to the average bro (e.g., KSM-66) are often very underdosed (and/or laced with impurities). Sometimes because of an outright scam, and sometimes because of incompetence by the manufacturer – I do not know which one is worse. In fact, most supplement companies usually only buy powder from China and then fill it into capsules or press it into tablets. As a side note, herbal supplements from overseas are a common cause of fulminant liver failure in ER departments.
Given all of this, it is a mystery to me why many people are wary of “big pharma” (which, for the most part, does not actively scam – only in rare isolated instances that are then blown up by the media), but are willing to inject an obscure white powder from the internet, which they know has been manufactured in clandestine conditions.
In sum, I have two major issues with peptides. Firstly, we know little about their efficacy and safety. Secondly, the likelihood that you are not injecting what you think you are injecting (e.g., identity, dosage, purity) is very high. The second point cannot even be disregarded for compounding pharmacies, which quite often are too incompetent to compound correctly (compounding peptides is quite hard actually and needs a lot of expertise in peptide chemistry to synthesize it, test it for the correct folding and sequence, purify it and then lyophilize it).
I personally feel comfortable experimenting widely with approved molecules (including peptides such as semaglutide or teriparatide which are manufactured by big pharma players) but, knowing what can go wrong, I am quite scared of peptides, more so if they are bought from obscure “research sites”.
Again, it may very well be that some peptides are perfectly safe and work the way they are touted to work. And that you are also getting a perfectly compounded (i.e., right AA structure & folding) and pure product. Nonetheless, the absence of credible knowledge in the face of injecting amino acid sequences is playing with fire.
If I had a billion dollars…
Kids are hypomanic at baseline. Meaning that they are energetic, usually in a great mood, capable of experiencing strong emotions, and highly curious. As kids grow older, the hypomania goes away. This has less to do with our archaic education system and more to do with changes in the brain. Dopamine levels decline, neuroplasticity declines, and presumably a plethora of other changes are happening.
What is it exactly that changes between “kid brain” and “adult brain”? I suspect that it could possibly be due to the differential expression of one, or likely multiple, key transcription factors – possibly TFs that govern neuroplasticity. For me, the days after doing ketamine I feel like a kid again, and it is known that ketamine activates a host of cascades, including gene expression changes, associated with neuroplasticity.
In bipolar disorder, during the (hypo)mania phase, the kid-like energy comes back. And usually the onset is quite sudden. Patients are usually driven, a charge of energy, and quite curious and eloquent (e.g., KeyTranscriptionFactor1 strongly downregulated) – even if before they were lethargic and depressed (e.g., KeyTranscriptionFactor1 strongly upregulated). During the “up” cycle of the disorder, many artists performed their greatest works during these episodes.
It begs the question whether the changes that are happening between “kid brain” and “adult brain” are also the changes that cause the “up” of bipolar disorder. Likewise, do the same changes but in the opposite direction happen in atypical depression? This is definitely a question worth exploring.
If so (which is hypothetical), is it possible to identify these transcription factors and possibly turn them on/off pharmacologically (or manipulate them via gene therapies)? If yes, that would not only be the ultimate treatment for depression, anhedonia, and mania but, given that there is a strong causal relationship between your biology and the extent to which you find life worthwhile, exciting, and meaningful, it may give us a tool to possibly recalibrate the human (biological) happiness setpoint to a higher level.
I, for one, would love to have a more “child-like” neurobiochemistry most of the time – full of fire, zest, and curiosity. If I had a billion dollars, hiring top researchers and exploring this question in depth would be among my top priorities.
It is probably healthier to take SGLT-2 inhibitors than to not take them
There are currently about 900 Mio. people (which is one in 9) living with chronic kidney disease (which simply means having poor kidney function that falls below a specific threshold – 60ml/min GFR). CKD is predicted to be the 5th most common cause of death in 2040.
The two most important things everyone can do to protect their kidney function are 1) control blood pressure (it does not matter whether with lifestyle or drugs) and 2) not be insulin resistant (which happens long before full-blown Type II diabetes). I discuss what antihypertensives (blood pressure drugs) to choose in an earlier weekly observation.
If you want to live into your 90s, you cannot have a GFR of 40ml/min when you are 70. The most nephroprotective drugs available are SGL2 inhibitors, which more and more lifestyle doctors have started to use quite liberally even in healthy individuals. They do not just protect the kidneys but also have unbelievable data in terms of heart health. Furthermore, they seem to be generally organ-protective and also reduce the incidence of cancer. For the vast majority of people, it is probably healthier to take them than to not take them. In the intervention testing program (ITP) canagliflozin increased median life expectancy by 14%. It also decreased the incidence of cancers across the board.
SGLT-2 inhibitors delay the time needed for dialysis by many years – the earlier one starts, the more potent the effect. As mentioned, the best way to protect the kidney is to control blood sugar and blood pressure – I discuss drug choices for these in an earlier weekly observation “Personal drug preferences for common conditions”. The best measures of kidney health are not creatinine but rather Cystatin C (blood test) and microalbuminuria (urine test).
What changed in 2024?
The drugs I currently take regularly are allopurinol, a low dose of hCG + finasteride, and weekly rapamycin. On most days of the week, I also take a single low dose of yohimbine as a short-term stimulant.
This year, I wanted to gain mass. Starting in April, I made it a goal to gain 1kg per month. I went from 68kg to 75kg over the course of 7 months. I gained both fat and muscle, probably to an equal extent. I feel and function much better with greater body mass, particularly greater fat mass.
Occasionally, I use nicotine gum (limited to 1h per day), low doses of psychedelics (about once per month to once every couple of months), and rarely ketamine (for anhedonic depression that happens every couple of months).
This year I have also experimented with pitolisant and NSI-189 and both molecules are promising to become a regular part of my stack. Pitolisant generally makes me more awake (without stimulating effects) and NSI-189 gives me vivid dreams, slightly stronger emotions, and a considerable libido boost.
This year, I also stopped a bunch of drugs I had been using for a long time. I stopped taking semaglutide half a year ago because it made gaining weight very hard. I also stopped taking metreleptin as I seem to have recovered from the after-effects of having had a very low body fat % at the beginning of my twenties. I stopped taking moclobemide because it seems to affect my cognition negatively – I tested this via Mensa IQ tests and it seems that on moclobemide my IQ is roughly 10 points lower. I stopped taking rasagiline because off the moclobemide I do not “need” it anymore as my dopamine levels are presumably quite high naturally.
I have exchanged the Huel for Yogurt drinks (Kefir). I still like to spike my drinks with olive oil and whey protein, giving me 900kcal per drink.
I still take a load of supplements but as far as I can tell they do very little to nothing – though I have been using them for 6-8 years now and no obvious harmful effects.
I discuss these and other changes in more detail in the “long version” What Changed in 2024?
Long-term appetite “rewiring” by semaglutide even after stopping?
In the past, I had been on semaglutide for 3 years. I tested out the whole dose range but the last 2 years I was only microdosing it (0.1-0.2mg per week – one to two clicks per day; daily is superior to weekly injections). Even on such a low dosage, I rarely had an appetite, particularly after adding a low dose of metreleptin. I am now off semaglutide for 10 months and off metreleptin for 3 months.
It feels as if would still be taking low doses of semaglutide and my appetite is mostly shot. I circumvent this partly by drinking high-calorie drinks (yogurt drinks spiked with olive oil) and eating a lot of nuts. Sure, I enjoy a good meal with friends but I do not enjoy the food itself very much.
I have become a very functional eater, simply because my food-induced pleasure is very low. I never think about food and I am rarely hungry. I actually quite enjoy this state because it “forces” me to get my pleasure from other, in my opinion more meaningful, sources. The major downside is that I have to ballpark calories & protein to hit my requirements.
Also another friend who had been on low doses of semaglutide for an extended period of time noticed something similar – despite being off the drug it feels as if he was still taking 30% of his semaglutide dose a year after.
Could it be that prolonged activation of “I am full”-pathways within the hypothalamus caused these circuits to long-term potentiate and thus strengthen? Analogously, if SSRIs are given, serotonin levels increase. Among other things, serotonin inhibits pathways within the amygdala, and the longer SSRIs are taken the weaker these circuits become. If one then stops taking the SSRIs, the altered connectivity and cytoarchitecture of the amygdala (and other brain circuits) is hypothesized to stay for a long time.
From the principles we know of the nervous system (“Use it or lose it.”; “Use it and develop it.”) the hypothesis that semaglutide leads to long-lasting changes in the appetite system seems not far-fetched.
I am aware that obese people gain most of their weight back once they stop GLP-1 agonists but their appetite centers were “broken” in the first place, and the hypothalamic inflammation associated with obesity may still be present. But what about healthy lean people with non-broken appetite centers? Nobody looked at the question.
From hormones to monoamines to ?
When I started out biohacking, I was all about hormones (and I still think that hormones are the most powerful molecules of all). Then, after experimenting with moclobemide, I realized that many of the effects I desired from hormones (e.g., greater energy levels & mood) can be had directly by messing with neurotransmitters – without exposing my whole body to hormones (as I mostly desired their effects on the nervous system). In other words, the focus changed from hormones to neurotransmitters.
After then having experimented with ketamine (which increased my energy and mood for weeks after the drug had left my body), I realized that there are very deep processes beyond hormones and monoamines, such as the gene expression changes that happen after ketamine or psychedelics or that happen naturally due to e.g., manic episodes, falling in love, or having found “purpose”.
There is something about intrinsic about the nervous system that we cannot target pharmaceutically. Is it mostly changes in connectivity? Large-scale changes in gene expression patterns?
This change from a more hormone-centered view to a neurotransmitter-centered view to a more “integrated(?)” view was one of the major changes in my approach to biological self-improvement.
Below are some examples I made in my article on mindset and top-down influences.
- A decade ago, I used to be semi-depressed for about half a year or so because I was reducing myself, my thoughts, and my feelings to molecular biology. Then, simply learning about the concept of emergence was quite powerful in terms of boosting my liveliness for months. In other words, I boosted my liveliness from “within” the mind. I am certain that the changes were quite real and not reducible to conceptual knowledge.
- The few times I fell in love with someone, I was always amphetamine-like stimulated for a couple of weeks, sometimes months. I was euphoric, needed less sleep, was less hungry, and had more energy. The neurobiochemical cascade of falling in love is characterized by higher levels of oxytocin, glutamate, and dopamine, among other things. Interestingly, falling in love is known to increase cortisol secretion by 40-100%. I am quite sure though that something „deeper“ than hormones and monoamines is also in place in the same way that mania cannot be fully explained by changes in hormones and monoamines.
- Before meeting my ex-girlfriend, I was in quite a bad place mentally. I was lonely, restless, and my “Urvertrauen” (trust in the Universe that things will be alright) was gone. I then saw somebody I was blown away by. On our first date, I knew that we would be a couple soon. After this single date, my Urvertrauen was restored and all the restlessness, loneliness, and unease, which had been there for months, was gone immediately, as if somebody had flipped a switch in my brain – even though my hormones or monoamines had presumably not changed much. This change in how I felt was holding up for months (as we got together). This was quite eye-opening to my bottom-up and biology- centered worldview.
- A couple of years ago, after one of my ex-girlfriends broke up with me, I was devastated for many months. In the same way that falling in love with her caused a hypomania-like state, losing her led to a state resembling true biochemical depression. The neurobiology of grief is thought to be characterized by an altered monoamine transmission and a dysregulated neuroendocrine control (hormones), among other things that are presumably even “deeper”.
A few more non-personal examples:
- The placebo effect is a prime example of a top-down effect. The placebo group in antidepressant studies usually measurably improves in a variety of domains. Similarly, being hopeful or simply believing in something can have measurable physio-biochemical ramifications.
- For many people, unresolved trauma can have massive effects on neurobiology, endocrine function, and physiology – sometimes for years.
- Children that are mistreated or neglected sometimes fail to thrive (to grow properly). This form of “psychosocial dwarfism” can occur even when adequate caloric intake is provided.
- In orangutan tribes (orangutans are somewhat closely related to humans), there is only one alpha male and something about the sheer presence of an alpha male has other male orangutans growth-suppressed (it is thought that his screams play a role). After the alpha male dies, the growth-suppressed young orangutans suddenly go through puberty. This means that puberty was induced from “within the mind”.
In all of these instances, biochemical changes are induced “top-down” (from within the mind) solely due to “information”. It is therefore not too far-fetched to claim that, for example, having a pessimistic or nihilistic mindset can sustainably alter monoamine transmission, hormones, and even “deeper” processes negatively (which then in turn favors a nihilistic or angst-ridden mindset).
(This is not to say that biochemical enhancement is not useful in finding purpose, love, or developing an optimistic mindset in the first place.) The main point of this entry is basically that vitality can be quite deeply affected by not just changes that are bottom-up (e.g., altering hormones or neurotransmitters through lifestyle or exogenous molecules) but also by more “psychological” changes (i.e., pure information), which eventually affect deep material processes within the brain, and presumably also within individual cells.
While this may seem “duh” to most people, for me, a biological materialist at heart, this was quite eye-opening to find out about – even though the biological mechanisms are far from being elucidated.
Neurobiochemistry & history
When I experiment with neuropharmaceuticals, my thoughts & outlooks change, which leads to a change in my behavior. Consequently, my personality changes. If I continued taking said neuropharmaceutical for life, my life trajectory would likely change. Similarly, the course of history changed majorly many times as individuals (or whole groups of individuals) altered their neurobiochemistry. A few examples:
- During WWII, a few billion methamphetamine pills were consumed by the Japanese, which amounts to hundreds of pills per person (including factory workers). Some historians believe that much of the country was on meth all the time, and this may have contributed to their reported “toughness” and aggression. For example, the brutality during the Rape of Nanking (300.000 people executed; roughly 50.000 rapes) as well as the bravery required for Kamikaze may have well been “influenced”. In sum, some historians argue, that the Japanese would not have behaved like the Japanese if it were not for methamphetamine.
- Dr. Theodor Morell, the primary physician of Adolf Hitler, experimented quite a bit. For example, numerous times, testosterone was injected into Hitler, including before major speeches or negotiations. Similarly, Hitler was quite fond of oxycodone (the active ingredient in OxyContin), which he reportedly loved as a “pick me up” drug. Of course, he was using amphetamine quite a bit as well. It is likely that Hitler and some others of the Nazi leadership had become meth addicts towards the end of the war. For a video about Hitler “tweaking”, see here. Some historians assume that some of their “grand” visions may have been amphetamine-inspired. Also, the German Blitzkrieg was methamphetamine-driven.
- Marc Aurel, the Roman stoic, was likely quite fond of poppy seeds (opium), which he reportedly consumed quite a bit. Similarly, Thomas Jefferson cultivated poppy seeds in his garden. I discuss the history of opioids briefly here.
- Reportedly, ISIS soldiers are strategically given tramadol (a weak opioid + SNRI) before battle and many ISIS soldiers are addicted to it.
- Some of the mass sacrifices of the Aztecs (up to many thousands per day on some festive days), may have been “influenced” by the use of cocoa drinks mixed with psilocybin-containing mushrooms. So much for psychedelics leading to moral progress (discussed here).
- When caffeine was introduced to the Western world, a lot of people started consuming it widely. Some historians argue that caffeine contributed significantly to the speed and extent of the scientific revolution, in part because people switched from drinking beer/ale in the morning (which was the go-to drink at the time because water was too contaminated) to drinking coffee, with significant societal impacts.
- JFK, who had an autoimmune disease affecting his endocrine system, reportedly took methyltestosterone (orally bioavailable testosterone), T3 (the active form of thyroid hormone), and prednisone (a more potent form of cortisol). However, he also took a host of drugs unrelated to his primary medical condition, including methadone (an opioid for pain), methylphenidate (Ritalin) and amphetamine, barbiturates (potent sleep drugs that have been taken off the market for their potency and abuse potential), and occasionally anti-psychotics for his mood swings. During the Cuban missile crisis, he reportedly was prescribed an increased amount of hydrocortisone and testosterone to help his “energy”.
Given my own experiences with how different molecules alter my behavior, I find substance (ab)use & history an incredibly fascinating topic – one that I think is highly underappreciated. I would particularly love to know what substance habits current prominent figures have – whether recreational drugs, stimulants, or antidepressants. I think we would be surprised.
What I created during these periods stayed
At times, my younger self used a bit of pharmacology to help him. For example, I wrote my thesis in six days. On one day of these six, I have taken 5mg of amphetamine. On this single day, I have written more than half of it. Similarly, six or seven years ago, strategic use of selegiline helped me make a decent amount of money, which I still profit from to this day. In the third year of med school, I used quite a bit of modafinil, which helped me to accumulate a lot of knowledge.
If one does this smartly, one does not necessarily need to make trade-offs with health. Even if one did (given these trade-offs are slight and temporary), for me, the tradeoffs were worth it because what I created during these periods stayed. Big caveat: to get net benefits from substance use, one needs to do this strategically and smartly. For the most part, recreational drugs (with few exceptions) are a net harm.
AGI may bring about “paradise engineering”
“The metabolic pathways of pain and malaise evolved because they served the fitness of our genes in the ancestral environment. They will be replaced by a different sort of neural architecture – a motivational system based on heritable gradients of bliss. States of sublime well-being are destined to become the genetically pre-programmed norm of mental health.”
Said in other words:
“Think of the most wonderful experience of your life – now imagine if life could be as good as that – or rather imagine if life could be better than that all the time. Just imagine if your best experience ever could be lower than tomorrow’s hedonic flaw. Other things being equal, wouldn’t it be better if we live in paradise?
Now, for much of history this kind of talk would be simply dismissed as utopian dreaming; that manipulating the environment in innumerable different ways has been tried and to be honest we’re not significantly happier now than ancestors on the African savanna – certainly not if suicide, depression marital breakup statistics etc. are taken seriously. However thanks to biotechnology now it will be possible re-engineer ourselves; to edit our own source code; to rewrite the vertebrate genome and to enjoy life animated by gradients of bliss.”
“Paradise engineering” is a term used by David Pearce to describe a world without suffering and where the vertebrate hedonic setpoint (going from -10 to +10) is lifted up by e.g., 100 points. Information is then identified by gradients of bliss (instead of negative and positive emotions).
When I hear people say “Next to extinction, the most likely outcome of AGI is a future of abundance” this kind of experiential abundance (rather than material abundance) is what comes to my mind.
While I am personally not 100% subscribed to David Pearce´s ideas, I will share some more of his ideas in a future newsletter because I think they are fascinating, thought-provoking, and also scary. In the meantime, I can recommend The Good Drug Guide – The Responsible Parent´s Guide to Healthy Mood-Boosters For All the Family. A tough read but worth it.
How to develop “super bones”
There is an unknown but powerful agent that has the potential to give every person great bone health. This agent is teriparatide.
Teriparatide is a synthetic analog of parathyroid hormone (PTH), which is important for regulating plasma calcium levels and bone metabolism. Continuously high levels of PTH are catabolic to bone but intermittently high levels (e.g., when given once daily), have potent osteoanabolic effects. In fact, PTH-analogs are the most potent bone-building molecules currently available.
Given that bone mass degenerates with age, often leading to fractures that eventually result in inactivity and sarcopenia, it makes sense to boost bone mass using teriparatide at least once after a certain age (e.g., 50 years).
Obviously, with very few exceptions every women should be on HRT after menopause (topic for another day). However, this is often not enough.
People shrink with age and their spine is subject to microfractures, causing back pain and functional impairment. Furthermore, after a femoral neck fracture (which is by no means rare), all-cause mortality rises by 500-1000% (even higher in frail individuals with comorbidities) during the first year and often remains close to double for the rest of the person’s life. One in three women and one in five men will have a hip fracture after age 50. While not as bad as femoral neck fractures, they are still associated with a 40-50% increase in mortality over 5 years.
Furthermore, given that mobility will be somewhat impaired forever after fracture (as old people have a hard time regaining muscles) this leads to a huge impairment in quality of life, for example, a reduction in walks, less social interactions, and a lesser ability to exercise. Which then leads to all sorts of secondary and tertiary consequences.
I worked with a university osteologist before and I asked him what he would do himself if he himself had osteoporosis. His response: 1) Take teriparatide for 2 years. 2) Do a single infusion of zoledronic acid (or oral alendronate for a couple of months) after teriparatide treatment ends to prevent some bone loss as after teriparatide the bone is in a state of increased remodeling resulting in a rapid bone loss upon cessation of teriparatide (only for a few months and by far not enough to make up for the teriparatide gains) – bisphosphonates prevent this state of heightened remodeling/bone loss.
However, this should not be just reserved for osteoporotic folks but can (and in my opinion should!) be done by every person after age 50. If every person did this after hitting age 50 or 55 I am sure that we would slash fracture rate by a decent amount.
I know a couple of people who used it (including myself but to recover more quickly from labral surgery). Other than some lethargy after injection initially (just use it at night!) nobody had any side effects. What are the risks? A tiny uptick in osteosarcoma barely worth mentioning – particularly if people only use it for 2 years. In numbers, the Forteo Patient Registry tracked about 100.000 patients and found only 5 confirmed cases of osteosarcoma which is barely higher than the general population (about 3-4 per million).
Teriparatide is synergistic with weight bearing in the same way that anabolic steroids are synergistic with resistance exercise.
Given access to the drug, this is how one can get a decent uptick in bone mass for decades to come. There is preliminary research that teriparatide also helps a little bit with cartilage tissue as it is supposed to have chondroregenerative effects – particularly peri-injury.
Muscular plasticity in adolescence
I know a number of people who are in their thirties and forties and look like they are on anabolic steroids. Except that they still have a full head of hair and their level of virilization (e.g., body hair) is low. All of them have great muscle definition and rather low body fat levels. All of them work out but not excessively.
Two of these are in their late forties, one was a wrestler and rugby player in his teens and the other was into bodybuilding at around the same age. The other person is now in their late twenties and was a track & field athlete during childhood and adolescence. While genetics certainly played a role that they went into these fields in the first place, I do not believe that genetics account for all of their current level of enviable muscular development.
The truth is, kids are quite “plastic”. This plasticity extends beyond just the brain (e.g., kids who are into chess/piano/soccer, etc. from early on will be better at it) and encompasses pretty much the whole organism.
People growing up at high altitudes do not just have higher hemoglobin levels, but every level of the organism adapts to the relative hypoxia. From an increased number of oxidative proteins, more abundant mitochondria, and presumably hundreds of other tiny low-oxygen adaptations.
Similarly, kids who are overweight in childhood will have a greater number of beta cells and thus higher insulin levels for life for any given carbohydrate load. Their adipocytes will also undergo hyperplasia (increase in cell count) instead of just hypertrophy (increase in cell size). This phenomenon is already observed in pregnancy – if the mother is overweight, blood sugar levels are higher, leading to a greater and more potent pancreas at birth and more fat cells (among many other things).
Similarly, when muscles are trained in a certain way from early on, more satellite cells will fuse thus leading to a greater number of myonuclei per muscle fiber. However, the adaptations likely go much beyond that – for example, the ratio of fiber types (Type I fibers – aka slow twitch fibers, Type IIa – aka fast twitch oxidative, Type IIb – aka fast twitch glycolytic) will be influenced via training, and so will the cellular protein machinery. Thus, if a person has the right genetic makeup combined with the right training at the right age, he or she can maintain great muscular development with comparatively little effort for life.
The only proven longevity supplement
The Intervention Testing Program (ITP) is a research initiative funded by the National Institute on Aging (NIA) to evaluate potential lifespan-extending interventions in mice. It is a program designed to test compounds that might slow aging and improve healthspan.
Lately, the ITP got more and more publicity – it is the best (and perhaps) only program in the whole world that can test the effect of compounds on health span and lifespan in a rigorous way. It is a multisite testing program, uses genetically heterogeneous mice, is blinded and controlled, and is also transparent with everything. Furthermore, after the mice die, their tissues and organs are histologically evaluated, something that is very rare in the field.
Notable successes are SGLT-2 inhibitors (14% lifespan improvement in males only), rapamycin (lifespan improvement depends on the dosage and sex but are on the order of 15-20% – the overall most consistent result), acarbose (22% in males and 5-10% in females), and 17-alpha estradiol (19% in males only). Notable failures were NMN/NAD+, resveratrol, and metformin (the ladder at least when not combined with other interventions).
The OTC supplement astaxanthin has increased male lifespan by 12%, which is a massive result. How does it work? We do not know exactly but it has been shown to modify multiple geroprotective genes including FOXO3 (common in centenarians), Nrf2 (a master regulatory transcription factor regulating the expression of antioxidant proteins), Sirt1 (we still do not know exactly what it does and how important it is in humans), and Klotho (helps with phosphate excretion through regulating FGF23 but seems to be implicated in all sorts of things).
Astaxanthin has shown fairly potent lifespan extension benefits in other species before but none of the experiments were, in my opinion, able to prove it in the way the ITP did.
Astaxanthin is the first widely available supplement that has been shown in the ITP to extend lifespan by more than 10%. Similar to other interventions (e.g., canagliflozin, acarbose, 17-alpha estradiol), it did not extend female lifespan. Why? We do not know.
Of note, astaxanthin is the reason flamingos, salmon, and shrimp are pink.
I personally take 12mg of astaxanthin per day. Given their (undeserved) popularity, I will touch on resveratrol and NAD+/NMN in more detail in a future newsletter.
From Long-COVID to Ironman training in 21 months
One of my best friends had gotten Long-COVID after his third COVID-19 infection. He was enjoying his life in Bali at the time. He had to pay 8000 euros out of pocket for a private Bali hospital stay for pretty much nothing. After a chaotic flight back in a wheelchair he moved back in with his parents and was housebound. Back then he could go for a single short walk around the block (but only on his good days). On his bad days, he was physically, cognitively, and emotionally wrecked and just lay around with brain fog.
For months, he slept 12-15 hours per day, had post-exertional malaise (energy crashes after increased activity), and had a host of psychiatric symptoms he never had before.
Interestingly, he was now also prone to bouts of anxiety, which he had never been before. He is the type of guy who goes out to the city and comes back home with three phone numbers from women he randomly approached on the street. Now he gets anxious when he is standing in the supermarket (which he rarely went to though). Often, he also got anxious and panicky before friends visited him and he usually kept visits to once per week only and only one person at a time. This heightened state of anxiety seems to be a common theme in the Long-COVID and ME/CFS community.
As he is one of my best friends, I wanted to help him but I could not, which made me feel quite helpless. Given that scientific progress was incredibly slow and nobody pretty much knew anything, I had to reason from scientific first principles and what was known at the time. We took matters into our own hands and after 4 months we started to experiment heavily.
Initially, our experiments were quite light but as time went on, we got more aggressive. The more aggressive we got, the better he got. Hard to say whether our experiments were causally related to his improvement – he thinks without a doubt.
Now, 18 months after getting the condition, he is back to resistance training and cardio. After 12 months, he approached 80-90% in everyday life but did not dare to exercise. Now, 18 months after, he is back to 100% in everyday life and roughly at 80% during exercise (hard to say though whether the exercise impairments are just due to the long period of inactivity). He is currently training for an Ironman, 21 months after getting long COVID.
Interventions with comments on what he thinks how important the intervention was:
- Pacing: He needed to avoid “crashes” at all cost. Thus, pacing himself was one of the most important aspects. Sometimes, he crashed for weeks after a single exertional event – particularly physically exertional things (such as going for a brisk walk). He also withdrew from stuff that was emotionally taxing (incl. meeting with friends if he did not feel like it). To make pacing easier, he took 10-20mg of propranolol (an unselective beta blocker that also penetrates the blood brain barrier) every day– bringing down both emotional as well as physical exertion. On his bad days and weeks, he also used benzodiazepines. Benzodiazepines brought down the anxiety and panic. While not optimal, our reasoning was that benzodiazepines are much less harmful than a crash. A lot of people were made worse (sometimes permanently) because their doctor thought that “graded exercise therapy” was a good idea.
- SSRIs: After starting escitalopram (gradual increase from 1.25mg to 10mg per day over the course of 1 month), things seemed to get better. The anxiety and panic were lessened and he had to use benzodiazepines much less. There is also quite a bit of evidence that SSRIs help long-COVID symptoms. He is taking 5mg of escitalopram to this day. In his opinion, SSRIs were a key aspect in helping him recover (whether that is true or not is hard to say). I discuss my experience with SSRIs here.
- Ketogenic diet: There is preliminary evidence that autophagy improves ME/CFS symptoms. A ketogenic diet gives about 70% of the autophagy benefits of a pure water fast (as insulin & IGF-1 levels are brought down to very low levels). He used a low dose of an SGLT-2 inhibitor (dapagliflozin 2.5mg) to make the ketogenic diet “easier” and more effective. Without the SGLT-2 inhibitors he was unable to reach ketosis for some reason, perhaps because he was so physically inactive at the time (which is terrible for insulin sensitivity). Theoretically, SGLT-2 inhibitors are contraindicated with a ketogenic diet but I feel combining them is perfectly fine if you know what you are doing. We just measured his blood ketone levels with urine sticks twice per day. Of note, supplementing with ketone esters is not even close to the same thing. It is not about ketosis per se but about the cellular adaptations (gene expression changes) associated with ketosis and plasma ketone levels are only a proxy for this. My experience with the ketogenic diet here.
- Fasting: He also did several 36h fasts, 72h fasts, and 5 day fasting mimicking diets. On fasting days, we stopped the SGLT-2 inhibitors. During times he did a lot of fasting, he got noticeably better. To make the fasting easier (without detracting from its effectiveness) he ate a lot of spinach and mushrooms and other very low-calorie foods that are filling up via volume. We did not do this all at once. We started with a ketogenic diet, after a couple of weeks we added the SGLT-2 inhibitors, and after 1-2 months we added the fasts. He is now back to a normal liberal diet (i.e., not watching his diet). Fasting is discussed here. My experience with fasting here.
- Everolimus: Right at the beginning we added 5mg of everolimus once weekly. Already after his first dose he could feel that something is slightly different (placebo?). This was one of our first interventions and he is taking the everolimus to this day (technically, he is currently taking rapamycin because of price and availability). We chose everolimus over sirolimus (rapamycin) because everolimus has a higher blood-brain barrier penetration. There is scientific evidence that anti-aging folks who have taken rapamycin before, during, and after a COVID infection have much lower rates of long COVID and their COVID cases are much milder in general. As an mTOR inhibitor, rapamycin leads to widespread changes in gene expression, downregulates the immune system, and reduces sterile inflammation. Inflammation is probably a key aspect of long COVID, particularly neuroinflammation.
- Valacyclovir: He used 1g/d of valacyclovir throughout (1 year in total). The idea is that ME/CFS is associated with the reactivation of herpes retroviruses (particularly EBV), and that this makes the neuroinflammation worse. Hard to say whether it helped or not. Of note, antivirals help some people with ME/CFS but not others.
- Ibuprofen: For a couple of months, he used daily ibuprofen (around 800mg per day). NSAIDs inhibit COX enzymes, which reduces levels of inflammation. He also used esomeprazole to prevent stomach ulcers. Celecoxib (COX-2 selective) would be a better choice because the risk of stomach ulcers is much lower and thus it does not need to be combined with a proton pump inhibitor.
- Metformin: The idea was to reduce levels of inflammation. He used 500mg twice daily for half a year.
- Ketamine: We did biweekly subQ injections of ketamine with a dosage of 0.5mg/kg. Ketamine increases neuroplasticity and reduces neuroinflammation. Frequent use is probably more neurotoxic than most people appreciate (discussed here), even at low doses. Nonetheless, we judged the effort-reward ratio to be favorable. Furthermore, he had been living without any form of excitement and pleasure for so long and the ketamine sessions gave him a much-needed emotional release. He did about 10-15 sessions in total.
- LDN: Low-dose naltrexone was a dead end. The initial week of anhedonia (naltrexone blocks the mu-opioid receptor – in other words, it is an “anti-opioid”) was highly uncomfortable. After 2-3 months he just stopped taking it because he felt like it did not do anything. This was also one of our first interventions because we judged the risk to be very low – but, as so often, so is the reward.
He claims that he could “feel” that every single interventions outlined above made him a tad better (other than the naltrexone). For most interventions, he could feel the changes quite fast (days to weeks). He had a couple of small setbacks associated with minor and major crashes. Initially (only taking low-dose naltrexone + everolimus) we did not know whether he is improving at all. However, he also did not seem to get much worse and so we stuck with everything and always thought about add-ons and improvements.
This protocol is quite extensive, aggressive, and not for the faint-hearted. However, in my opinion, it touches many different angles that may be etiologically related to the development and persistence of long-COVID. We argued that the risks associated with this protocol are less than the risks of doing nothing.
Anyway, he is mostly back to normal now and has his old life back. He is exercising again, leading his small company, and leisure travels quite a bit.
Whether the self-experiments were the cause of his getting better or whether he would have gotten better anyway on his own is impossible to tell. However, the temporal correlation and the fairly rapid improvement (months) suggest a causal relationship. At the very least we can say that the experiments have not prevented a recovery from happening and no interventions seem to have made him worse.
Speculating on the origins of Elon Musk’s impulsivity
Over the past couple of years, Elon Musk seems to have become much more impulsive. While there are many possible explanations and while this may even be part of a strategy (“Even bad publicity is good.”), this may also be due to neurobiological changes. Surprisingly, I have never seen anybody mention this hypothesis before.

Elon Musk has mentioned on multiple occasions that he has a prescription for ketamine (for reported depression) and doses “a small amount once every other week or something like that”. He has multiple tweets about it. From personal experience, I can say that ketamine can make some people quite hypomanic for a week or so after taking it. Furthermore, ketamine is quite neurotoxic – far more neurotoxic than most doctors appreciate (discussed here). So, is Elon Musk partially suffering from adverse cognitive changes from his ketamine use? If he has been using ketamine for multiple years, this is at least possible.
A lot of tech bros, such as Jeff Bezos, are on TRT. I would not be surprised if Elon Musk is as well. TRT can make people more status-seeking and impulsive due to the changes it causes to dopamine transmission. However, TRT – particularly at normally used doses – is far from sufficient to cause Elon level of impulsivity.
Elon Musk has seemingly also been experimenting with amphetamines (here), and he probably also has experimented with bupropion, which he says is “way worse than Adderall and should be taken off the market.” Adderall (amphetamine) and bupropion, which is an amphetamine derivative are both known to increase impulsivity.
Elon Musk claims to also be on semaglutide (Ozempic). While Ozempic may decrease impulsivity due to its effect on the reward system, it at least shows that Elon has little restraints about intervening heavily into his biology.
In this cherry-picked clip (link) he seems quite drugged to me, particularly due to the way his uncanny eyes seem unfocused. While there are many possible explanations ranging from overworked & tired, impatient and wanting to get back to work ASAP, mind-wandering, Aspergers, etc., recreational drugs are an option. The WSJ has an article on Elon Musk using recreational drugs at least occasionally (link).
Whatever the case, I personally think that Elons change in personality is at least partly due to neurobiological intervention. Whether this includes licensed pharmaceuticals or involves recreational drugs is impossible to tell. I am confident that most lay people are heavily underestimating how certain interventions can change a personality.
While this is only a wild guess, the only molecule I know of that can cause sustained and severe increases in impulsivity are MAO-B inhibitors such as selegiline or rasagiline. Selegiline is also licensed as an antidepressant with the name Emsam. I know about half a dozen people who have experimented with MAO-B inhibitors and everyone notices a drastic (and sometimes even destructive) increase in impulsivity. Given that selegiline is prescribed by some “unconventional” psychiatrists to help with productivity, such as the doctor of Sam Bankman Fried (FTX), I would not be too surprised if Elon is using it as well – particularly in line with his seemingly drastic change in behavior.
An alternative is the irreversible MAO-inhibitor tranylcypromine, which seems to be more commonly used for depression nowadays. It was the only substance that ever put me into a sustained hypomania. In my opinion, MAO-B inhibitors (selegiline, rasagiline) or irreversible MAO-inhibitors (tranylcypromine) would be sufficient to explain the personality changes of Elon Musk. This is pure speculation however and there are surely many other explanations as well. I describe my own personal experience with selegiline in this week’s article here.
Whatever the case, Elon seems to have changed and changes to his neurobiology may be causally underestimated. As Sam Harris says: “I have been quite amazed at Elon’s evolution, both as a man and as an avatar of chaos. … If Elon is still the man I knew, I can only conclude that I never really knew him.”
Why do I biohack?
There are probably a number of different explanations, depending on the angle.
- From a biological perspective, I would argue that my dopaminergic tone is quite high and I am just inherently curious. For some reason, I found biology particularly interesting, particularly the applicable aspects of it, and I have a lot of fascination regarding applying this to my life.
- From a personal/egocentric perspective, I would argue that I self-experiment so much because I want to “maximize” the only life I can be sure of having in this universe. Given that I found out about the incredible influence biology has on the subjective (well-being) and objective aspects of my life (life trajectory), I want to optimize the biological domain as much as possible (and I want to help others do the same).
- From a psychological/psychotherapeutic perspective, one could argue that I want to make myself “better” because for a long time I have had a deep-seated feeling of not being ”good enough the way I am naturally”. This may stem from being yelled at a lot for little reason throughout my childhood, elementary school bullying (as I moved to a different elementary school at the age of 8 I was bullied for 4 years for no reason), and a feeling of “inferiority” because of my former lack of height.
- From a rational/”mathematical” perspective, I believe that the potential rewards of finding something that makes my life “better” for years to come outweigh the costs & risks of intervening. Biohacking then just becomes a rational choice that, over the long run, pays a lot of dividends.
Rectification regarding rapamycin & infections
In a previous eail, I mentioned that rapamycin might have caused an infection after laser treatment. However, that conclusion may have been premature and incorrect. It seems the real issue was not rapamycin but the local subcutaneous diffusion of imiquimod to the lesion sites, which triggered inflammatory processes and delayed wound healing. I had been using imiquimod to treat a handful of water warts at distant sites.
I found multiple similar experiences on Reddit, and three dermatologists I consulted confirmed that this scenario is plausible.
The lesions began to subside immediately once I stopped using the imiquimod cream at other sites plus applied some betamethasone (a potent glucocorticoid). I also ended up on antibiotics for no reason!
(I still think that imiquimod is a super fascinating molecule!)
Imiquimod is an amazing molecule
Applying the cream twice on a water wart caused my immune system to attack and destroy it within a couple of days.
Imiquimod is a TLR7 agonist. Toll-like-receptors are pattern recognition receptors that detect foreign stuff. If they are activated, this alerts the immune system to attack.
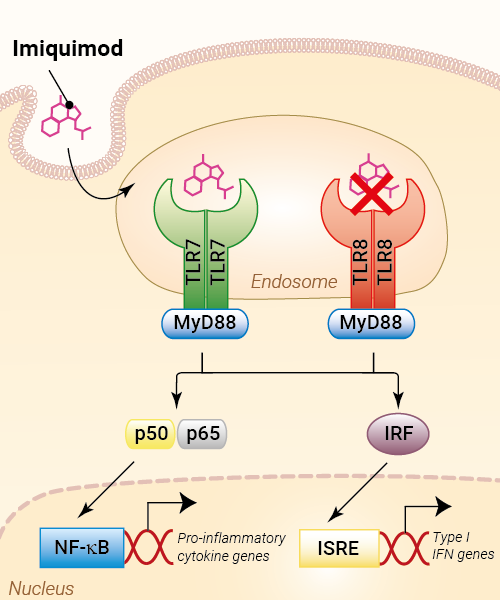
Topical application of imiquimod is quite effective at treating all kinds of warts (e.g., HPV warts, water warts, etc.) and even some skin cancers.
Related to this, immunotherapy is presumably the only silver bullet against cancer because it may be the only thing that can take out micro-metastases throughout the body (solid metastatic organ cancer is deadly almost 100% of the time). I wrote an article about cancer immunotherapy: Here.
Edit: Imiquimod is not so amazing after all. It is what caused the “infections” discussed in a previous newsletter. Imiquimod stimulates inflammation and it seems that dermal application can provoke inflammatory reactions even on distant wounds. Funnily, the scar on my shoulder (which is at the opposite site of my body) turned red while I was applying imiquimod in my groin area.
My battle with molluscum contagiosum
I got infected with molluscum contagiosum, which is a mostly harmless but incredibly annoying virus. The virus replicates in the superficial layer of the skin, leading to the development of water warts, which are harmless but infectious.
I probably got infected back in December and it took me a long time to realize that these “ingrown hairs” were not ingrown hairs after all.
My immune system was weakened back then by a bout of COVID-19 (which is known to mess up the adaptive arm of immunity for a long time to come). The fact that I am on rapamycin probably did not help either as it is immunosuppressive. Alternative hypothesis: God punishes my promiscuity and sends me a fair warning.
I immediately went to a friend, who is a dermatologist and had them removed with a CO2 laser. Two weeks later, the lesions had healed to a point where one could not see them anymore, other than some slight hypopigmentation.
However, a couple of new water warts had appeared. Enter CO2-laser round #2. On the same day, I took 2mg of rapamycin (which I had paused since January) because I wanted to check my sirolimus peak plasma levels in the hospital laboratory. Lo and behold, all of the lesions got infected, four of them quite nastily.
Unfortunately, the infection was resistant to cephalexin (a cephalosporine antibiotic). Bacterial infections are one of the most common side effects people notice on rapamycin. I was flabbergasted by how just 2mg of rapamycin took out the innate arm of my immunity.
(I have been on rapamycin for 5 years and this is my first infection. The only thing that changed between laser round #1 and round #2 was the introduction of rapamycin.)
Edit: These were not infections after all…but enhanced inflammation caused by imiquimod cream – discussed in a later observation.
Amputations at 45? Everyone should get an lp(a) test!
As part of my rotations, I am currently working at a ward for cardiac and vascular surgery. There are lots and lots of amputations happening all the time. When patients are lucky, it is just a toe. But most of the time, it is the whole foot or lower leg.
Most of the patients have a combination of long-standing poorly controlled hyperglycemia and full-time smoking. The endothelial inflammation and the neuropathy lead to non-recognized and poorly healing infections which may eventually turn into sepsis – hence the preemptive amputation.
This week, however, there was a lower leg amputation on a guy who is barely 45 years old. He was not overweight and did not have diabetes. While he was a smoker, the primary reason for losing his lower leg at such a young age was elevated levels of lp(a).
In his case, the elevated levels of lp(a) led to early atherosclerotic degeneration of blood vessels, including manifest peripheral artery disease. A small injury led to a poorly healing infection, which turned into the requirement for amputation.
Lp(a) is an insidious particle that is much more important than commonly appreciated. About 10% of people have genetically elevated Lp(a), which may have conferred an advantage in blood clotting in the past. Again, evolution favored something that is awesome for the young at the expense of the old.
Fortunately, my Lp(a) is naturally low (around 15mg/dl). If my Lp(a) were high, I would turn to PCSK9 inhibitors to lower it. There is also an antisense drug on the way that will hopefully be available for clinical use soon (pelacarsen).
Hormones can be replaced for life without adverse effects, if they are replaced well.
Recently, I saw a patient who was 81 years old and she was taking 150mcg of thyroxine (T4). She had been on this dose for over 30 years because of total thyroidectomy. Her TSH is completely suppressed and had been this way for decades. She felt “phenomenal” (actual quote), was quite lively, did not need blood pressure or lipid-lowering medication (perhaps due to her higher levels of thyroid hormones) and was definitely healthier than most other 80-year old patients.
Similarly, I recently had a patient who had a six-pack at 75 years of age. He was type I diabetic and had been replacing his insulin since he was 14, meaning that for 60 years he had been relying entirely on exogenous hormone replacement to survive. Other than the insulin and pantoprazole, he did not use any other medication. He was quite vital, had a full head of hair, and exercises every day. Compared to most other Type I diabetics, he uses only very low doses of a basal insulin (20IU per day) and primarily uses walking and exercise as his primary method of controlling postprandial glucose excursions.
The point I am making is not that these people may have gained an advantage because of their exogenous hormone replacement (which may or may not be true) but rather that, given that hormones are replaced well, one can replace them for life without obvious adverse effects – such as these two individuals, who were relying to 100% on exogenous thyroid hormones and insulin respectively for multiple decades.
Many people I meet are of the opinion, that exogenous hormone replacement must be bad because it is “artificial” and “natural” is better. However, our human bias for preferring “natural” may lead us astray. The artificiality of intervention is not per se associated with “you will eventually pay for your sins!”
Low-dose insulin experiment
My life is a biological laboratory and I am constantly running experiments, some of them “work” but most of them fail. However, almost every experiment teaches me something, such as the experiment done over the last two weeks.
For years, I kept my insulin sensitivity very. For example, when I eat a candy bar (for science), my blood glucose is back to baseline, and often even below baseline, after already 30 minutes. I attribute this to my low levels of body fat, strategic exercise, and metabolic hacks, including GLP-1 and leptin manipulation.
However, a consequence of high insulin sensitivity is low basal levels of insulin. Because little insulin is required to maintain blood sugar at a healthy level, little is secreted by the pancreas.
Despite of what all the “influencers” in the sphere are preaching, insulin is not exclusively bad. Sure, it drives the mTOR pathway (and therefore aging) and hyperinsulinemia is associated with all kinds of chronic diseases, such as cancer, dementia, and atherosclerosis.
But as so often, the dose makes the poison. Insulin is similar to insulin-like-growth factor 1 (IGF-1). Both of these are anabolic hormones, perhaps the most anabolic hormones known to mankind.
Insulin is also responsible for driving glucose and amino acid into cells, inducing them to be active. Furthermore, as a medium-term satiety peptides, it gives a “go-ahead” signal to the hypothalamus that the organism has plenty of resources to use for activities besides acquiring food.
When “the hormone of abundance” is very low, such as in type I diabetes, individuals basically “wither away”, both mentally and physically – in part because their cells stop metabolizing nutrients and enter a kind of “conserve resources mode”.
A normal physiological production of insulin is about 60 IU per day, 30 IU as a basal insulin (constantly trickled into the blood stream) and roughly 30 IU in response to eating food (prandial production of insulin).
So, what would happen if I, say, add 5 IU of a long-acting insulin to my physiology? Presumably not much because that would only slightly elevate my total insulin. Wrong. Even such a low amount of insulin significantly increased my energy levels and mood – particularly on day 1 and day 2. And the change in how I felt was quite striking. Furthermore, my heart rate variability (as measured by my Oura ring) decreased by about 10 points and my resting heart rate at night increased by 5 points (from about 45bpm to about 50bpm).
All of these changes are indicators that my sympathetic nervous system activity increased. After 10 days, I then stopped the insulin injections and on that day I felt tired, “weak” and moving around was particularly onerous. The changes in resting heart rate and HRV reversed – indicating that my sympathetic nervous system output had dropped again.
I also got lightheaded multiple times, presumably because my CNS had partially adapted to the higher SNS-activity, analogous to how people feel tired and weak after having taken simulants for a couple of days and then suddenly stopping.
I then reintroduced 5 IU of insulin degludec and lo and behold, my SNS activity rose again.
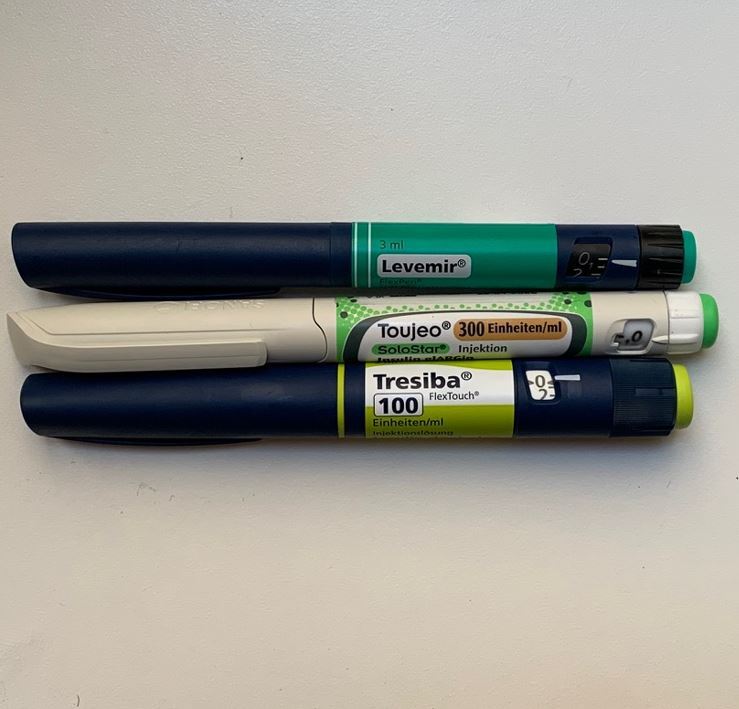
Lessons #1: My basal insulin levels are very low – perhaps too low.
Lesson #2: While having very low levels of insulin may be good for longevity, it may not be optimal for vitality. As so often, vitality and longevity are at odds.
Lesson #3: Insulin degludec had more pronounced effects that insulin glargine or insulin detemir – 3 different forms of long-acting insulins that differ in their half-lives and presumably also in their ability to cross the blood brain barrier.
“TRT lite” without being shut down
I recently started taking a low dose of hCG to specifically elevate my levels of estradiol, which are particularly low due to carrying little body fat (body fat expresses aromatase – and the more fat one carries, the more testosterone aromatizes into estrogens, particularly estradiol).
I have been doing this for 4 months now. I am currently on a dosage of 70 IU per day. On this dosage, both my E2 and T levels are decently higher than they would normally be, in the 800s ng/dl and 30s pg/ml respectively. More surprisingly, my HPTA is not shut down and both my LH and FSH are still in range.
Lesson: By doing daily injections, one can do a “TRT lite” without being shut down. Not being shut down makes coming off a non-issue as LH and FSH will be back to their normal levels within maybe a week or so.
Conversely, the longer (and harder) one is shut down (e.g., by using more suppressive androgens and/or higher dosages), the greater the risk of having issues with recovering properly, presumably due to epigenetic modifications in hypothalamic neurons.
I´ll publish an in-depth experience report about my second round of testosterone experimentation soon.
Edit: A year after having started this experiment (and liking it), I wrote an article about my experience: For more: My TRT Lite Protocol
My Background
I hold an MD and am currently in residency. My clinical and academic interests primarily lie in endocrinology and psychiatry. However, I am currently on the path to becoming a general practitioner, as I am not fond of the clinical practice of these specialties. Eventually, I plan on having my own practice (probably with a good friend who specializes in laboratory and sports medicine), focusing on longevity, health span, vitality, life-enjoyment, cosmetic endocrinology, cognitive performance, and everything tangentially related to these.
Updated every couple of months. I usually write two of these observations per week and send them out via my weekly newsletter.
